Esophagogastric varices are dilated blood vessels that develop in the esophagus or stomach because of portal hypertension (high pressure in the veins that deliver blood to the liver). They do not cause symptoms unless they rupture and bleed, which can be life-threatening. If someone has varices that bleed, they should go to the emergency room right away.
The causes of esophagogastric varices vary by person, but the most common causes are scarring (cirrhosis) and high blood pressure in the portal vein system. People with cirrhosis are more likely to develop esophagogastric varices than people with other types of liver disease. Other causes of portal hypertension include blood clots, right-sided heart failure and parasitic infection called schistosomiasis.
Liver diseases
Symptoms of esophagogastric veins include difficulty swallowing or breathing, pain in the chest or back when swallowing or coughing, and a change in the color of your stools. You may also feel nausea or a full feeling in your abdomen.
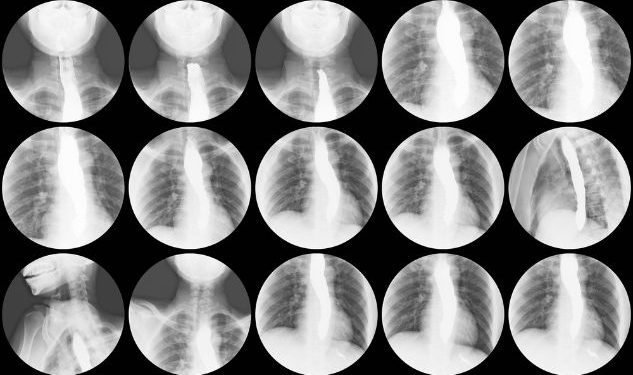
If you have esophagogastric varices, your doctor may recommend an endoscopy to see the inside of your upper digestive tract. An endoscope is a thin, flexible tube with a camera on the end that is inserted through your mouth and guided down to the esophagus and stomach. The camera sends images to a monitor, which the physician can use to detect enlarged veins that might be causing bleeding.
Other tests to diagnose esophagogastric varices are X-rays and CT scans. These tests provide pictures of the liver or blood flow in the liver and allow the provider to identify enlarged veins that might be causing esophagogastric varices and a risk for bleeding.
Bleeding esophagogastric varices
If someone has bleeding varices, they will have bloody vomit or black stools, or both. The person may also have a fever or other signs of illness, or they might not be able to eat or drink.
During treatment, your doctor will try to stop the bleeding using medications to slow the blood flow in the portal veins and divert it away from the varices. They may also place a shunt between the varices and the portal vein to relieve the pressure and prevent bleeding.
They may also put elastic bands on the varices to tie them off and prevent them from leaking blood. The person may also be given a steroid or other medication to reduce inflammation in the varices.
Other treatments are non-selective beta-blockers to decrease blood flow in the portal veins and a procedure known as transjugular intrahepatic portosystemic shunt (TIPS). This technique places a stent between the liver and heart, which decreases the pressure in the portal veins and stops the bleeding.
Another type of treatment is injection sclerotherapy, where drugs are injected into the varices to create a blood clot that blocks blood flow through the varices. This method is often effective but can produce severe complications, such as bleeding into the esophagus.
If you have esophagogastric veins that are leaking blood, your doctor will suggest an endoscopy and begin treatment to stop the bleeding and prevent further loss of blood. This can be done with rubber bands or by injecting a blood clotting agent into the varices. Your doctor will also give you medicine to help with the discomfort caused by the leaking blood and a prescription for antibiotics to prevent further infection.