Decompression sickness symptoms, also called the bends, are a dangerous condition that can develop among scuba divers when they decompress too quickly. DCS is caused by nitrogen dissolved in the blood and tissues that forms bubbles when pressure decreases rapidly (e.g., during ascent from a dive or while leaving a compressed air environment).
Symptoms of decompression sickness may appear within minutes or hours after decompression begins. They can be severe or mild.
The most common symptom of mild to moderate decompression sickness is pain in the joints and muscles. It can occur in the arms or legs, but it may also involve the back and tendons. It usually occurs as a throbbing or aching pain that worsens when moving, such as when stepping or walking.
If the symptom is more severe, it can lead to organ damage, which can be permanent or even fatal. Other symptoms can include numbness, weakness, difficulty speaking or dizziness, and difficulty breathing.
Early treatment with high-flow oxygen from a cylinder can relieve symptoms of decompression sickness and sometimes prevent it from developing. However, this should not be done unless advised to do so by a medical professional trained in dive medicine.
Avoid diving for two weeks to a month after experiencing any symptoms of decompression sickness. If the symptoms do not subside, return to the surface immediately for a doctor’s evaluation.
Get a complete medical history before diving. This includes a review of your diving history, dive times, ascent rates, surface intervals, and breathing gases. Ask your doctor about any symptoms you experienced during a previous dive or during your current dive.
Consider any pre-existing heart or lung diseases, such as high blood pressure or a history of asthma. People with asthma or other lung conditions can have thin-walled air pockets in their lungs known as bullae that do not empty quickly when they exhale, which can cause problems after decompression.
If a person’s bullae rupture, he or she could become ill from a pulmonary barotrauma (collapsed lung). This can result in a pneumothorax, which requires emergency treatment with a chest tube to drain the air.
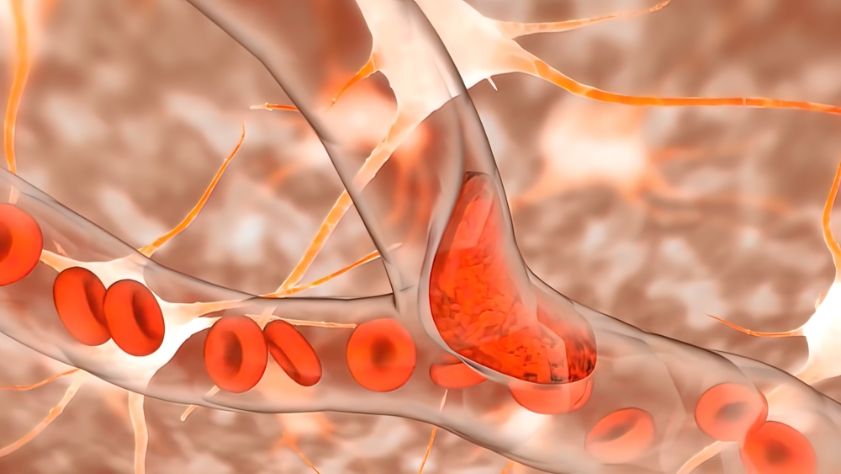
A collapsed lung can cause a blockage of many of the small blood vessels in the body. This can cause pain or other symptoms, such as numbness or weakness on one side of the body, difficulty speaking or dizziness, and trouble breathing.
The resulting blood vessel blockage can also trigger blood clots, which can be fatal or cause long-term disability. Fortunately, these symptoms typically resolve quickly after being treated with high-flow oxygen.
Those who have a severe form of DCS or an air embolism, such as a pulmonary barotrauma, should not return to diving until they have been evaluated by a medical specialist. These patients may need to be hospitalized for several days if they have a collapsed lung.
If the symptom is severe, it can lead to organ damage, including a heart attack or stroke. Other symptoms can include numbness, tingling, arm or leg weakness, unsteadiness, vertigo, or difficulty breathing.









