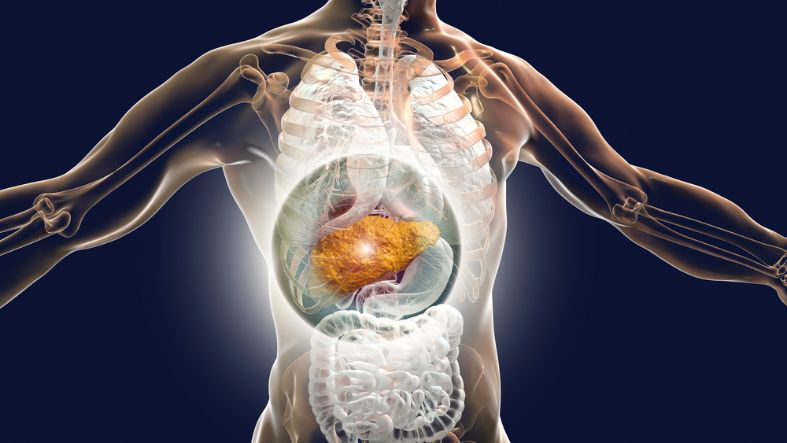
Hepatocellular carcinoma (HCC) is the most common primary liver cancer, accounting for 70 to 90% of all HCCs. The incidence and mortality of hepatocellular cancer is increasing worldwide, with an estimated 200,000 new cases expected in Europe by 202012.
Although HCC is often associated with chronic liver disease ranging from viral hepatitis to non-alcoholic fatty liver disease (NAFLD) and NASH, it can occur even in the absence of cirrhosis. Several factors may promote the development of HCC in non-cirrhotic livers, including obesity and diabetes mellitus.
The underlying genetic causes of HCC are complex and involve a dynamic sequence of molecular and epigenetic changes that accumulate over time. The alterations may include genomic amplification of mutations, aberrant DNA methylation and chromatin acetylation, as well as changes in mRNA expression levels of key tumour genes and inflammatory mediators. These changes may be caused by a combination of chronic liver disease-related oxidative stress, inflammation and fibrosis.
Hepatocellular carcinomas develop in a stepwise fashion, starting with dysplasia and advancing to neoplastic growth as livers become damaged from metabolic, oxidative and inflammatory damage. These processes generate an environment that is conducive to carcinogenesis and result in a spectrum of heterogeneous hepatocyte phenotypes with distinct growth characteristics and prognostic characteristics.
Inflammation is a major pathogenic factor in HCC, with chronic inflammation associated with NAFLD, NASH and NASH-related HCC. The inflammatory process in NAFLD results in a derangement of hepatocyte fatty acid metabolism and increases the production of reactive oxygen species, which cause oxidative stress. The inflammatory response is also accompanied by increased expression of cytokines and chemokine receptors, which stimulate hepatocyte proliferation and hepatic cell death.
Insulin resistance and the metabolic syndrome are other important risk factors for the development of NAFLD-related HCC. Insulin resistance is a hallmark of the metabolic syndrome and is associated with increased glucose and insulin concentrations, decreased plasma antioxidant capacity and higher insulin secretion. The metabolic syndrome can also increase hepatocyte fatty acid oxidation and the production of reactive oxygen species. This in turn, can lead to hepatocyte inflammation and DNA damage.
Various anti-inflammatory and immune-modulatory approaches have been developed to reduce inflammation in the liver, owing to their therapeutic properties and their ability to alter the course of liver disease and hepatocellular carcinoma. The aim of these strategies is to decrease oxidative stress and inflammation, while promoting hepatocyte regeneration and repair of liver tissue.
Hepatocytes are sensitive to oxidative stress and inflammation as well as a range of other stressors, such as chronic liver disease-related fibrosis and hepatitis C virus infection. Besides inflammation, hepatocytes are also vulnerable to apoptosis in response to DNA damage and oxidative stress. These mechanisms are likely to be responsible for the high HCC risk in patients with hepatitis C virus infection.
Liver transplantation is the most common curative treatment for HCC. The success rate is generally high, with a 5-year survival of 70-80%12.
Surgery remains the cornerstone for curative treatment, with hepatectomy and lobectomy, or liver resection and transplantation, being the preferred methods in the United States. However, some guidelines recommend ablation in early-stage small tumours, mainly in hepatocellular carcinomas that are not suitable for resection due to their location, size or multi-nodularity12. Image-guided ablation uses chemical, thermal and electrical techniques to direct a targeted injury to the tumour. These methods have become increasingly popular as they are safer, more precise and less invasive than surgical procedures. They can be performed in a single session or in a series of sessions and are generally used as an adjunct to resection for patients with hepatic dysfunction.









