A dermatologist can diagnose basal cancer cells through a biopsy. This type of skin cancer typically develops in people over 50. However, it can also occur in younger people who have extensive exposure to the sun. The good news about basal cancer is that it generally has a slow growth rate and rarely spreads to other parts of the body. However, it’s still important to have regular skin checks to ensure that there are no changes that indicate cancer.
The UC xenograft model confirmed the presence of basal-like cells at the tumor-stroma interface. Immunohistochemical staining revealed that these cells had low levels of CEACAM6. Furthermore, immunohistochemical staining of normal urothelium revealed a similar pattern. Basal cells of urothelium contained no CEACAM6 protein, whereas intermediate and superficial cells were readily identifiable.
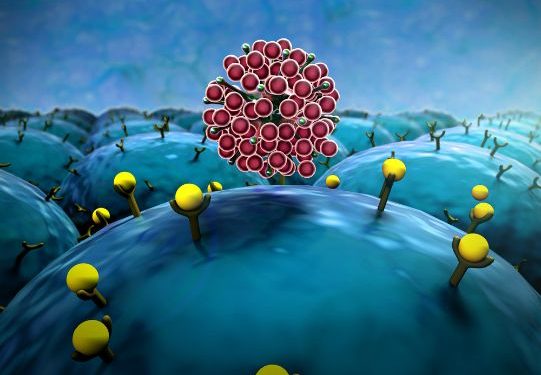
The pharmacological inhibition of CCR5 inhibits the growth of basal cancer cells. Specific antagonists inhibit the pro-invasive and metastatic functions of CCR5.
Besides its anti-tumor properties, MELK inhibits growth of both luminal and basal breast cancer cells. However, it has side effects in some patients. It may be harmful to normal cells, so this treatment is currently not suitable for all patients. In this case, MELK inhibition may be a good option. If this treatment is successful, it may be able to stop cancer cells while maintaining normal tissue. This would be a good treatment for basal-like breast cancer.
Xenograft studies were conducted in accordance with National Institutes of Health guidelines and the Dana-Farber Cancer Institute’s approval protocols. Mice were NCR-nude. The cells were resuspended in 40% Matrigel-Basement Membrane matrix (MBM) containing LDEV-free cells. Mice were anesthetized with isoflurane and injected with up to 5 x 106 cells per site. Tumor growth was monitored using calipers.