In 1997, Bonnet and Dick showed that cancer stem cells were present in nonobese diabetic/severe combined immunodeficient mice. Since then, many solid tumors have been identified as containing cancer stem cells, including breast, lung, colon and melanoma. Researchers are now seeking to understand how cancer stem cells initiate cancer and what they can do to help. Here, they discuss the latest research and answer questions about cancer stem cells.
In the meantime, scientists continue to develop ways to help people fight cancer. One approach is to use induced pluripotent stem cells, which are derived from the cells of already-born humans. These stem cells tend to accumulate cancer-causing mutations. These mutations can pass on to the final cell, which is why they carry the risk of developing cancer. Cancer-stem cells are not as effective as tumor-specific therapies.
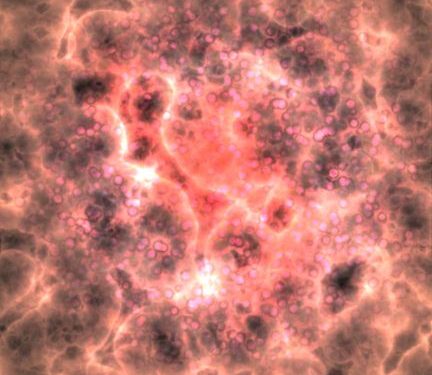
Current treatments for gliomas are geared towards the active proliferating cells present in the tumor mass. GSC-oriented approaches are promising in overcoming resistance and lowering the risk of recurrence. These methods eliminate the quiescent cells present in tumors, and eliminate the cellular crosstalk with non-stem cancer cells. However, these therapies have not been shown to work on gliomas due to the resistance to immunotherapy.
While the concept of cancer stem cells is not entirely new, it represents a paradigm shift. Several scientists have studied tumor-initiating cells in human cancer and discovered that they are characterized by their ability to self-renew and differentiate. When transplanted into other people, cancer stem cells can become tumors and spread throughout the body through a process known as metastasis. For more information, please visit the website below.
A clinical trial is underway to test the effectiveness of cancer stem cells in humans. UC Davis researchers identified these cells in 2007 and published their findings in the Journal of Neuro-Oncology. A study by the UC Davis neurosurgery department led by Dr. Rudolph Schrot and Dr. Joyce Ma developed a new therapeutic agent for cancer stem cells and is now testing it in laboratory animals. There are also other stem cell lines being studied in clinical trials, and these are also being tested for human use.
The traditional theory of cancer stem cells states that tumor-initiating cells are a minor subpopulation. They maintain a low level of mitotic activity, which protects them from treatment approaches designed to target cells that are actively dividing. The low mitotic activity of CSCs may contribute to cancer recurrences. But it does not explain all aspects of cancer. If successful, this theory will help us understand some of the mysteries of cancer.
The PD-L1 gene has been shown to overexpressed on breast CSCs, which may be a consequence of increased stemness-related pathways. Activation of this signaling pathway by Wnt inhibitors inhibits PD-L1 expression, while Wnt activators had the opposite effect. In other cancers, PD-L1 has been shown to be present in putative cancer stem cells, including lymph node metastases and tumors. Additionally, CMTM6 is implicated in upregulation of b-catenin and a process that expands the pool of cancer stem cells.