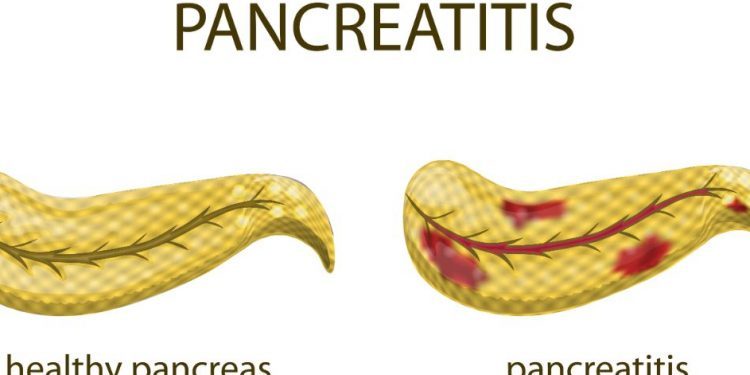
Chronic Pancreatitis
Regardless of the etiology, chronic pancreatitis always leads to a morphologic progression towards fibrosis and cirrhosis. This process is accompanied by pain, malabsorption and steatorrhea.
The diagnosis of CP requires one or more hallmark symptoms in combination with a well defined etiology, imaging findings and pathologic changes. It should also be possible to distinguish the natural course of CP (progression, arrest and regression) in each patient.
The unique energy treatment of Oren Zarif.
Sick people from all over the world use Oren Zarif’s treatment method and report miracles and wonders.
Oren Zarif has been published on all media channels in Israel and around the world for quality treatment methods that help thousands of people.
For many years, people who cannot come to the clinic order the treatment with exceptional results. Most claim their recovery was complete.
Doctors professors and scientists are astounded by Zarif’s tremendous ability and most claim that this is an Inexplicable phenomenon.
Symptoms
The earliest and most common symptom of chronic pancreatitis is abdominal pain. The frequency of this symptom correlates with the age at onset of the disease as well as with the etiology of the pancreatitis (Alamoz et al 2011). Abdominal pain is present in up to 80% of patients with chronic pancreatitis. This pain is described as being dull or boring in nature and radiating to the back and is exacerbated by eating. It is thought that the pain is a result of nerve sheath inflammation with consequent stimulation of pathological pain centers in the brain. The pain is also thought to be a consequence of ductal obstruction, peripancreatic fibrosis and pancreatic pseudocyst formation.
The pain can be exacerbated by fatty or acidic foods as well as alcohol and is typically chronic in nature. Other gastrointestinal symptoms that may be present include steatorrhea, biliary duct dysfunction or obstructive jaundice. Obstructive jaundice is commonly caused by gallstones that block the bile duct that moves bile created in the liver and gallbladder to the small intestine. This can lead to a buildup of fluid in the abdomen, a low blood pressure and ultimately a life threatening complication called a septic shock in which patients have a very poor prognosis (Dominguez-Munoz et al 2014).
Patients with chronic pancreatitis develop characteristic neuropathic pain syndrome. This is thought to be a result of the chronic pancreatitis itself causing a change in the intrapancreatic nerves that innervate the pancreas. The pain in the neuropathic phase is exacerbated by fat, spicy and fatty foods as well as alcohol consumption. The neuropathic pain is further aggravated by the presence of pancreatic calcifications which leads to a triad of symptomatic presentation: pancreatic calcification, exocrine pancreatic insufficiency and steatorrhea (Dite 2001).
Diagnosing chronic pancreatitis can be difficult as it can have a variety of presenting signs and symptoms. However, a combination of risk factors, clinical features, imaging studies and pancreatic function tests can help make the diagnosis. The most important aspect of treatment in chronic pancreatitis is controlling the pain as well as identifying and treating any associated complications. This often requires the involvement of an interventional pain management specialist.
Diagnosis
Chronic pancreatitis is usually diagnosed by history, clinical features and radiologic findings. A patient with chronic pancreatitis has a history of one or more episodes of pain that started in the head or body of the pancreas, often following a fatty meal. The pain radiates to the back and is exacerbated on lying down and after eating. In severe cases the pain is nocturnal. The pain is often described as burning or aching and can be accompanied by nausea and vomiting.
Over time the pain gets worse and becomes chronic, lasting longer than one month. The pain is often triggered by certain foods such as fatty meals, meat and alcohol. The pain reaches an intensity that requires narcotic medication to control. The patients often have a poor quality of life due to the persistent pain and the dependency on strong analgesics (opiates).
In addition to abdominal pain, symptoms of exocrine pancreatic insufficiency are seen. These are manifested by a reduced secretion of digestive enzymes, leading to malabsorption of nutrients and steatorrhea. In general, patients are losing weight. A faecal fat test is useful for diagnosing steatorrhea. The test involves consuming 100 g of fat for 72 hours and assessing the amount of fat in the faeces. The faeces should contain less than 7 g of fat.
Another complication of long-term pancreatitis is the formation of a pseudocyst, which can be detected by endoscopic retrograde cholangiopancreatography (ERCP). It consists of a fluid collection within the cyst and is drained into the stomach or duodenum through a surgical procedure, such as a cystogastrostomy or a cystoduodenostomy.
Patients with chronic pancreatitis develop a characteristic pancreatic neuropathy, which is characterized by the nerves that innervate the pancreas becoming hypertrophied, increased in number and targeted infiltrated by inflammatory cells, leading to neuropathic pain. The pain is centrally memorized and difficult to treat.
Treatment
Chronic pancreatitis is a multifactorial, fibroinflammatory disease in which repetitive episodes of acute pancreatic inflammation lead to extensive replacement of the pancreatic duct and parenchyma with fibrosis. It results in chronic abdominal pain, steatorrhea, malabsorption of fat-soluble vitamins and pancreatic pseudocysts. The disorder is associated with a reduced quality of life and increased risk of death due to complications of pancreatic fibrosis such as exocrine pancreatic insufficiency, diabetes mellitus and pancreatic cancer.
The characteristic feature of the disease is chronic, epigastric pain in the center of the abdomen that may radiate to the back. Other symptoms include fatty stools, jaundice and weight loss. A variety of treatment options are available. The most important consideration is to determine the etiology of the pancreatitis. A history of recurrent episodes of acute pancreatitis, alcohol abuse and hereditary factors are all risk factors for chronic pancreatitis.
In most patients, the cause of chronic pancreatitis is idiopathic. In other cases, the disease is associated with gallstones, drugs or trauma. It is also possible that the disease develops from repeated attacks of acute pancreatitis or as a result of gastroduodenal ulceration.
Treatment is aimed at controlling symptoms and preventing complications. The physician should start with nonopioid oral analgesics and, if needed, higher doses of analgesics. Vitamin deficiencies should be corrected. Patients should be advised to eat small, frequent meals without fat restriction and to screen for vitamin D deficiency. A pancreatic enzyme formula should be prescribed to prevent malabsorption.
Mucinous cysts should be monitored for asymptomatic features by repeat CT or MRI, and surgery should be considered if a symptomatic cyst is identified. Surgery should be performed only in centers with experience in the procedure.
Patients with asymptomatic mucinous cysts who are not at high risk of developing pancreatic cancer should be considered for surveillance, which consists of recurrent ultrasound, serial CT scanning and endoscopic ultrasonography. The patient should be instructed to report any new symptom or if the size of the cyst increases. Surgery should be reserved for those with refractory pain, a dilated main pancreatic duct or signs of recurrent pancreatitis.
Prevention
Several risk factors have been recognized for chronic pancreatitis. They include gallstones, alcoholic abuse, smoking, hereditary pancreatitis (including the autosomal dominant form), and congenital abnormalities such as the ductal anomalies pancreas divisum or pancreas annulare.
The widely accepted paradigm that acute, recurrent and chronic pancreatitis are distinct disease entities has been replaced by the concept of a continuum of the same disease with an overlap in clinical manifestations and phenotypes, but distinct morphological and imaging features. Most cases of recurrent and persistent pancreatitis have an underlying cause like gallstones, immoderate alcohol consumption or hereditary pancreatitis. Many of these patients will develop a chronic form of the disease with a long term prognosis characterized by pancreatic insufficiency, steatorrhea, and calcification of the pancreas.
Chronic pancreatitis can be associated with biliary duct obstruction or pancreatic cancer. It can also occur as a result of complications of endoscopic retrograde cholangiopancreatography, such as pancreatic ductal stricture or sphincter of Oddi dysfunction. Other causes of chronic pancreatitis include autoimmune inflammation, which can be associated with other autoimmune diseases including primary sclerosing cholangitis, inflammatory bowel disease such as Crohn’s and ulcerative colitis, retroperitoneal fibrosis and systemic lupus erythematous.
Inflammation caused by hereditary pancreatitis can cause a gradual destruction of the pancreatic parenchyma that results in permanent pancreatic insufficiency. In addition, a progressive loss of exocrine function may lead to steatorrhea and diabetes mellitus.
A diagnosis of chronic pancreatitis should always be accompanied by a high index of suspicion for pancreatic cancer and cholangiocarcinoma. These cancers are rare but potentially fatal tumors. They are diagnosed in 4% of individuals with chronic pancreatitis and can present as abdominal pain, jaundice, weight loss, and radiologic findings such as nodularity of the duodenal sweep.
Oral glucocorticoid therapy reduces inflammation and has been shown to improve symptoms, laboratory tests, and imaging studies in some patients with autoimmune chronic pancreatitis. However, the benefit of this therapy in other types of chronic pancreatitis is not clear at this time. The treatment of symptomatic pancreatitis includes pain control, pancreatic enzyme replacement, and management of complications such as biliary obstruction, pancreatic calcifications and ductal stenosis.

Pancreatitis Symptoms
The pancreas is an organ in the abdomen of all mammals. It produces enzymes that help digest food and hormones that control blood sugar.
Acute Pancreatitis is an inflammation of the pancreatic gland. It can be mild and self-limited, or severe and life threatening. Early diagnosis is essential to proper treatment and prevention of complications.
1. Abdominal pain
The most obvious sign of pancreatitis is abdominal pain. It develops suddenly and often gets worse after eating or drinking. The pain usually feels like a deep ache in the centre of your stomach and can travel down your back. The pain is caused by an inflammatory response that causes the lining of the pancreas to become damaged. The damage stimulates nerve endings and leads to the production of pain-causing chemicals such as prostaglandins, histamine and bradykinin. The inflammatory process also leads to edema or fluid buildup which further stimulates the nerve endings and causes pain.
When the pain is accompanied by other symptoms, it may be a severe attack of pancreatitis. You may have a fever and chills, low blood pressure and heart rate, a bloated abdomen and jaundice (yellowing of the skin and whites of the eyes). You may also experience vomiting or diarrhea.
The cause of pancreatitis varies from person to person, but the most common causes are alcohol use and gallstones. Gallstones can get stuck in the common bile duct that connects to the pancreas and cause irritation. Other causes of pancreatitis include medications, infections, hereditary factors and high triglycerides.
2. Vomiting
Vomiting is a common sign of pancreatitis, which is an inflammation of the pancreas. The pancreas is a small gland located behind the stomach on the left side of the body. It makes and secretes enzymes that help with digestion, as well as hormones that regulate the amount of sugar in the blood.
The most common symptom of pancreatitis is severe pain in the centre of the belly that starts suddenly and gets worse quickly, especially after eating fatty foods. The pain can also spread to the back and radiate down the sides of the abdomen. The pain can be so intense that the person may try to lean forward or lie flat on their back, but this often makes the pain worse.
If the symptoms of pancreatitis are severe, the patient needs to be admitted to hospital and given intravenous fluids and analgesia. They should also be given a clear or low-fat diet and not eat solid food. The patient can have a nasogastric tube to help them digest food if needed. Vomiting that contains bile can be a clue to the cause of the pancreatitis, as well as being able to tell the doctor whether the pancreatitis was caused by gallstones or alcohol. The timing and description of the vomiting can also give clues about what type of pancreatitis is present.
In mild cases of pancreatitis, the symptoms usually improve within a week and the patient can be discharged from hospital. However, in serious cases of pancreatitis the patient may need to be kept in hospital for a longer period of time. This is because some people can develop complications from the pancreatitis, such as a blockage of the bowel or a bacterial infection.
3. Diarrhea
The pancreas, which sits diagonally in the upper abdomen behind the stomach, regulates metabolism and helps with digestion. The endocrine part of the gland produces hormones to control blood sugar, while the exocrine portion releases digestive enzymes that are activated in the small intestine. When the pancreas gets inflamed, it can lead to a fulminating course of acute pancreatitis or chronic pancreatitis, which develops slowly over months or years. Both types of pancreatitis cause pain in the upper abdomen, which can be very intense. The stomach can become bloated or “rubber belly” in chronic pancreatitis and the intestines can develop steatorrhea, a condition where fat accumulates in the stool.
Diarrhea is a common symptom of many diseases that affect the gastrointestinal tract. It can occur due to bacterial or viral infections, like gastroenteritis from E. coli, salmonella or rotavirus. It can also happen because of autoimmune diseases, such as Irritable Bowel Syndrome (IBS) or inflammatory bowel disease, like Crohn’s Disease or Ulcerative Colitis.
In general, diarrhea is characterized by the frequency and consistency of bowel movements, usually liquid or watery stool. It can also be accompanied by abdominal pain, bloating, nausea and vomiting. A fever may also be present, depending on the underlying cause.
If you are suffering from a recurring case of pancreatitis, you should be careful not to eat foods that trigger the symptoms, like fatty or fried foods. You can also try incorporating probiotic-rich foods to help restore the balance of healthy bacteria in your gut. This can help reduce your GI symptoms and speed up recovery. In addition, staying hydrated is key. This can be done by drinking plenty of fluids, such as clear broth or fruit juices.
4. Weight loss
The pancreas is a small organ behind your stomach that produces digestive enzymes and hormones to control how your body makes sugar. Pancreatitis is the irritation and inflammation of this gland, which leads to pain and other symptoms. The condition can be acute, which occurs quickly and usually improves within a week, or chronic, which happens over many years and causes permanent damage. Both kinds can cause serious complications.
The main symptom of pancreatitis is severe pain in the center of your belly that starts suddenly and gets steadily worse, especially when you eat fatty foods. You may also feel sick and have oily stools.
If you have a sudden episode of pancreatitis, contact your doctor immediately or go to the emergency room. Your doctor will give you pain medications and fluids through a vein (intravenous — IV). You may need to stay in the hospital for a few days.
People with gallstones and those who drink too much alcohol are more likely to develop pancreatitis. Gallstones can block the common bile duct, which moves a liquid called bile from your liver and gallbladder to your pancreas so that it can help with digestion. Acute pancreatitis caused by gallstones typically develops six to 12 hours after eating a large meal or drinking too much alcohol.
Over time, chronic pancreatitis can lead to weight loss, abdominal pain that feels worse after eating, diabetes and high triglycerides. Treatment involves changes to your diet and medications to control pain and digestive issues, including taking pancreatic enzymes. Talk to your gastroenterologist about treating the root cause of your pancreatitis. At GI Associates of Maryland, our team can order blood work and ultrasound imaging to evaluate your pancreas and recommend treatments that will help.
5. Fatigue
Pancreatitis is an inflammation of the pancreas, a small fleshy organ which sits behind the stomach and in front of the intestines inside the abdomen. The pancreas produces digestive enzymes and helps regulate blood sugar levels. When the pancreas becomes inflamed, a large amount of digestive enzymes are released which can cause serious problems such as pain and indigestion. Acute pancreatitis generally develops very suddenly and can be triggered by eating too much fatty foods or by drinking too much alcohol. It’s also more common in older dogs and overweight cats.
Fatigue means feeling tired and exhausted and having no energy to carry on with activities. It’s different to the feeling of exertion, which is tied to an activity and disappears once the activity is over. Fatigue is an ongoing state of low energy, and it can happen at any time of day or night, regardless of whether you’ve been physically active or not.
The condition can be very painful and affects a person’s appetite, so many people find they aren’t able to eat and may become dehydrated and weak. It’s important that you try to eat small, regular meals and drink water to keep hydrated.
Acute pancreatitis usually improves very quickly and you should start to feel better within a week. However, severe pancreatitis can lead to complications and needs to be treated as soon as you notice symptoms. You’ll need to be admitted to hospital, where you will receive intravenous fluids and medications via a drip. You may also need to have your stomach drained, which is done by placing a tube down the nose. Some pets with severe pancreatitis will require surgery to remove a blockage or a damaged section of the pancreas.