Diabetes can cause many different foot problems, such as ulcers and foot infections. These can be painful, debilitating and lead to amputation.
The best way to prevent these problems is to get your blood sugar under control and see a podiatrist regularly. The ADA recommends that people with diabetes have a hemoglobin A1C test at least twice a year.
Glucose is what your cells need for energy. Normally, your body makes and uses insulin to help glucose get into your cells. When you have diabetes, your body doesn’t make enough insulin or use it properly. This means that glucose doesn’t get into your cells as quickly as it should and causes high blood sugar levels, which can lead to diabetic foot symptoms.
Diabetic foot symptoms can vary from mild numbness and tingling to intense burning pain. Most of these symptoms are caused by nerve damage and poor circulation.
Changes in your skin: Dry, cracked and peeling skin on your feet is a common sign of nerve damage. A doctor can apply a moisturizer or lotion to your feet to help them recover. This can be painful and difficult, but it’s important to do so.
Calluses: People with diabetes develop calluses more often than people without diabetes. If they’re really thick, a provider can cut them down to reduce the risk of infection.
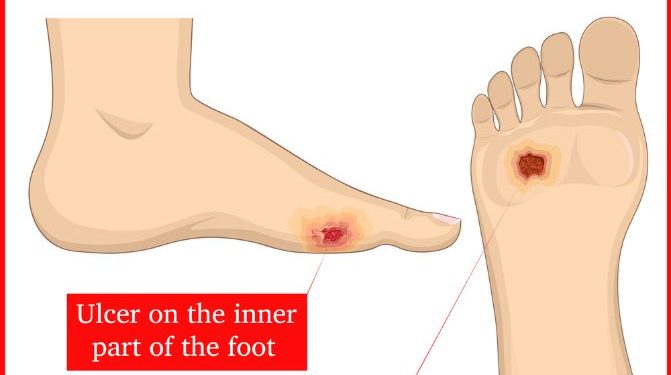
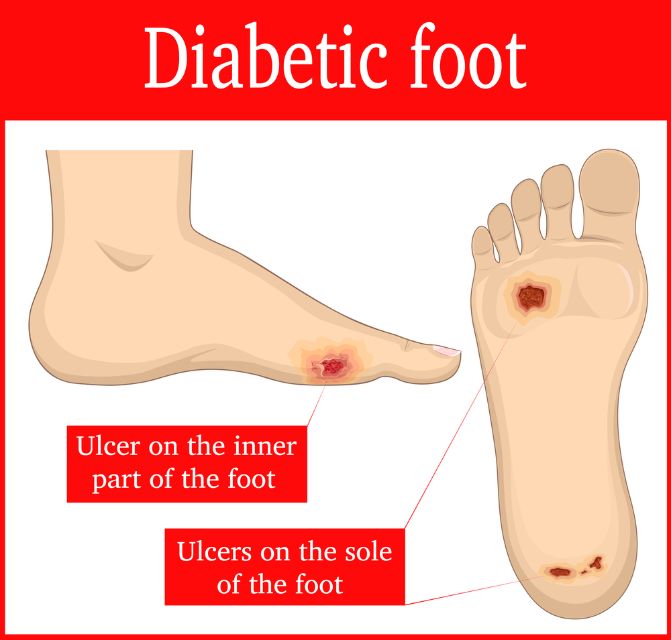
Ulcers: If a person has an ulcer, it needs to be treated by a provider right away. If an ulcer is left untreated, it can become infected and spread to the rest of your foot or leg. This is why all ulcers need to be seen by a provider.
Charcot foot: If a person with diabetes has weak bones in their feet, they can break. This can happen suddenly or slowly over time. If it goes untreated, the break can change your foot’s shape. It may look like the arch of your foot has collapsed into a rocker shape.
If your foot is swollen, red, and warm, you should get it checked out by a doctor. This is usually a sign that you have diabetic neuropathy, which can cause numbness and pain in your feet.
Your doctor will want to know about your health history, including your hemoglobin A1C, and any history of wounds or infections in your feet. They will also check the skin, muscles, and bones in your feet to look for signs of circulation issues that can make it harder to heal a wound.
The exam will also include looking for any sores or blisters that haven’t healed. If you have a new sore, your doctor will likely elevate your foot to help it get better.
Treatment for diabetic neuropathy is usually done by a podiatrist or a doctor who specializes in caring for feet. A doctor can administer an injection of medications into your feet, or use other treatment options, such as physical therapy and heat therapy.
Pregabalin (Lyrica): This is a medication that’s used to treat diabetes-related nerve pain. It can be taken 2 to 3 times a day, and it’s typically recommended by podiatrists because it can ease nerve pain.