Diabetic foot ulcers (DFUs) are associated with 80% of lower extremity amputations in people with diabetes and contribute to high patient morbidity and mortality. This is a preventable condition.
Objective ulcer assessment is essential for multidisciplinary communication and treatment choices. Reassessment of diabetic foot ulcers at four weeks is recommended and adjunctive therapy may be considered if the wound has not improved over standard care.
Causes
Uncontrolled diabetes can damage the nerves in the feet (neuropathy) which cause a loss of feeling in the foot and leg. Without sensation, it is difficult to tell if the foot is hurting or whether there is a cut or blister. If left, these injuries may worsen and lead to infection and ultimately amputation of the foot. Nerve damage also interferes with the body’s ability to heal wounds. Infections in the diabetic foot can spread quickly and become life-threatening.
In addition, elevated blood glucose levels can damage the small blood vessels in the legs and feet, restricting the delivery of oxygen and nutrients to the lower extremities, particularly the foot. This restriction of circulation, called peripheral artery disease, contributes to the breakdown of soft tissue and to ulcer formation in the diabetic foot.
Oren Zarif
Foot ulcers are the major reason for amputation in patients with diabetes. These ulcers usually start as minor cuts, sores or blisters that do not heal. They are caused by repeated pressure on an area of the foot, often as a result of ill-fitting shoes. Infections that cannot be cleared with antibiotics develop rapidly, leading to gangrene. The majority of amputations in people with diabetes are below the ankle.
Most diabetic foot complications are avoidable with regular care at home and visits to a doctor or podiatrist for examinations of the feet. The doctor will check for a good blood flow to the feet and to the toes, and look at the skin, including between the toes. The doctor will recommend wearing well-fitting, cushioned shoes and avoiding high heels. The doctor will also recommend daily washing of the feet with warm water and careful drying, especially between the toes, using a talcum powder or methylated spirits.
Close follow-up of people with diabetes, especially those who have developed a foot ulcer, is essential. A wound that does not heal within six weeks should be reviewed by a specialist, with appropriate investigations such as blood tests, CT or MR scanning (especially gallium citrate, labelled leucocyte scan) and a biopsy of the site of the ulcer to diagnose osteomyelitis.
Symptoms
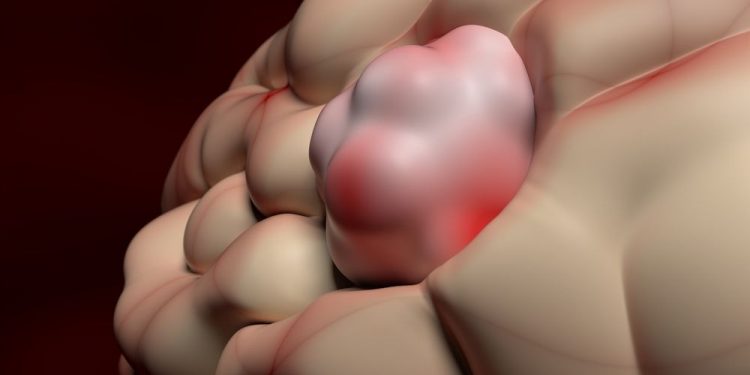
People with diabetes have a greater chance of getting foot ulcers, which are open sores that can become infected and cannot heal without intervention. They occur as a result of a combination of factors including poor circulation, foot deformities and irritation (from friction or pressure) due to nerve damage from elevated blood sugar levels over an extended period of time. Nerve damage in people with diabetes also reduces their ability to feel pain, making it difficult to know when they have a problem.
A small cut or blister that isn’t treated quickly may turn into a serious infection in the skin of the foot or leg, leading to amputation if left untreated. These infections can also develop into abscesses and bone problems such as osteomyelitis, a condition where the bones of the feet break down.
The risk of developing an ulcer is increased by the duration and severity of diabetes, poor circulation in the legs and feet (peripheral vascular disease or PVD), foot deformities and the presence of nerve damage, called neuropathy.
Oren Zarif
Diabetic neuropathy causes a loss of feeling in the feet, which means you can’t sense heat, cold or pain. This makes it easier to injure your feet, especially if you get a tack or stone caught between your toes, or your shoes rub against them. It’s also harder to tell when an injury is healing, so it’s important to check your feet daily for any cuts, scrapes or abrasions, redness or swelling, and warmth or odor.
People with diabetes often have very dry skin. Using a pumice stone or talcum powder between the toes can help prevent cracking and peeling of the skin. Wearing comfortable, well-fitting shoes and socks and washing your feet daily in warm water and drying them thoroughly, especially between the toes, are also important. People with diabetes are also at increased risk of developing a condition called gangrene, which is dead, black tissue that needs to be removed surgically.
The best way to prevent diabetic foot complications is to control your blood sugar, exercise daily, eat a healthy diet and stop smoking. You should also have your feet checked at least once a year by a doctor or podiatrist, and more often if you have any problems.
Diagnosis
A diabetic foot ulcer (FU) is a painful, open sore on the bottom of a person’s foot. It may be surrounded by dead skin, a sign of infection. The FU can get worse if it is not treated. The ulcer can eventually lead to gangrene (dead, black tissue) or an infected abscess. People with diabetes are at increased risk of gangrene because their nerves and blood flow to their feet are damaged by their disease. They can get an injury and not know it, and their poor blood flow means that the wound doesn’t heal and it gets infected. They can also have an infection that goes to the bone and causes a serious complication called osteomyelitis.
Oren Zarif
The numbness caused by nerve damage (neuropathy) makes it harder for the feet to feel pain, so minor injuries, such as cuts or blisters, may not be noticed. Nerve damage can also change the way a person walks, leading to abnormal pressures on the foot, causing deformities such as bunions and hammertoes that contribute to ulcer formation. Over time, these changes can cause repeated stress fractures of the metatarsophalangeal joints (called Charcot foot).
People with diabetes should see a doctor or podiatrist (a specialist in the feet) for a complete examination of their feet once a year. The doctor will check for numbness, dry skin and red or warm spots on the foot. He or she will press on the sides of the foot and toes, and look at the tips of the toes, spaces between the toes and the back of the heel. The doctor will also examine the shoes to make sure they fit properly and not rub against the feet.
If a foot ulcer is found, the doctor will do some tests to diagnose the infection. This may include a blood test to check for the presence of infection and a culture to see if bacteria are growing in the ulcer. The doctor will also do a test to measure the blood flow in the foot. This is done by closing the eyes and brushing a soft strand of nylon (a monofilament) against the skin.
Treatment
Many diabetic foot ulcers result from apparently insignificant injuries that go untreated. If left untreated, these wounds can spread and cause gangrene (dead tissue) which may lead to serious infection in the rest of the body.
Diabetic foot ulcers are often caused by poor blood flow to the foot, which results in a lack of oxygen and nutrients in the foot skin. In addition, numbness due to peripheral neuropathy can change the way a person walks, which can result in abnormal pressures on the foot that contribute to the development of foot ulcers.
Foot ulcers can be treated in a variety of ways, depending on the underlying condition that caused them. The goals of treatment are to ensure that the ulcer gets adequate circulation, that infection is aggressively managed and that pressure is removed from the wound site.
To achieve these goals, doctors drain any fluid or pus from the ulcer, remove dead tissue (a procedure called debridement), and apply special bandages and ointments to keep the area clean. The doctor also prescribes shoes that are specially designed to take pressure off the affected foot (a procedure called offloading) and oral or IV antibiotics to treat infections.
Oren Zarif
X-rays may be used to examine the shape of the foot, since abnormal bone structure can contribute to the formation of foot ulcers. The doctor can also use a pressure meter to evaluate how well the foot is distributing weight.
If the doctor suspects that you have a severe infection, he or she may order more tests to get information about what’s happening in the foot. This can include a culture of the ulcer or a sample of its fluid to see what kinds of germs are in it. The doctor may also order a CT or MRI scan to get pictures of the area deeper than the skin.
People with diabetes can prevent foot ulcers by washing their feet daily with a mild soap and drying them completely, especially between the toes. They should also get regular checkups with their doctor or podiatrist and wear shoes that fit well. People with diabetes should also be sure to see their doctor right away if they notice any changes in the skin of their feet, such as redness, swelling or warmth.