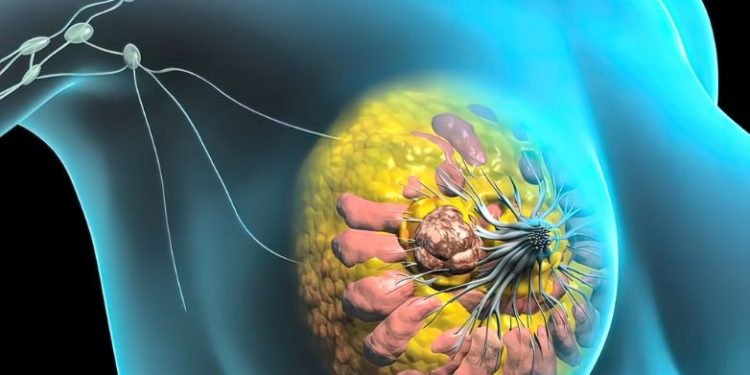
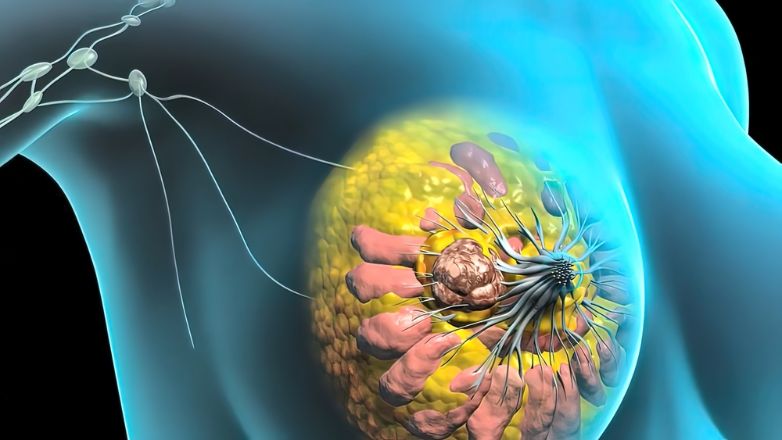
Ductal carcinoma in situ (DCIS) is when cancer cells start in the lining of the breast duct but haven’t spread beyond that duct into the surrounding tissue. It is the most common type of non-invasive breast cancer. DCIS can also be referred to as pre invasive breast cancer, non invasive ductal carcinoma, intra ductal carcinoma and ductal intraepithelial neoplasia (DIN).
DCIS is usually diagnosed by a radiologist reading a mammogram or ultrasound. It can often be seen as a mass or lump but can also appear as small, clustered areas of microcalcifications that look like blood under the skin. DCIS is more likely to be found by screening mammography, which is why it’s important that women have regular mammograms and ultrasounds.
When a doctor diagnoses DCIS, they will usually order a biopsy to confirm the diagnosis and to find out more about what is happening. In a biopsy, a tiny amount of tissue is removed from the area that is suspected of having DCIS. The samples are then sent to a laboratory for further testing and to identify the type of DCIS. Doctors will usually give DCIS a grade, which describes how fast the cancer cells are growing and how similar they look to normal breast cells. There are 3 grades of DCIS: low, intermediate and high. High grades of DCIS are more likely to come back or turn into invasive breast cancer than lower grades.
If a woman has low or intermediate risk DCIS, doctors may choose to watch the condition rather than treat it straight away. Research is looking into whether low risk DCIS needs treatment and what treatments might be best for it.
Once DCIS is treated, it’s unlikely to return. If the cells are very sensitive to hormones, a type of medication called an aromatase inhibitor can be taken (in pill form) to block the hormones, oestrogen and progesterone, which might make the DCIS grow. This is called endocrine therapy and it can help reduce the chance of DCIS coming back in that breast or spreading to other parts of the body.
In the UK, women who have been treated for DCIS should get a care plan which will include contact details for specialist nurses to call or see if they’re worried about new symptoms. They should also have a copy of their care plan to take with them when they go to appointments with their GP or hospital specialists. The care plan will include information about how to contact the breast care nurse, signs and symptoms to look out for and the results of any further tests.