Getting the call from your doctor telling you that your pap smear results came back with atypical endometrial cells can be scary. After all, you might think that it means you have cervical cancer. But it is important to understand what these atypical cells mean and what steps you should take next.
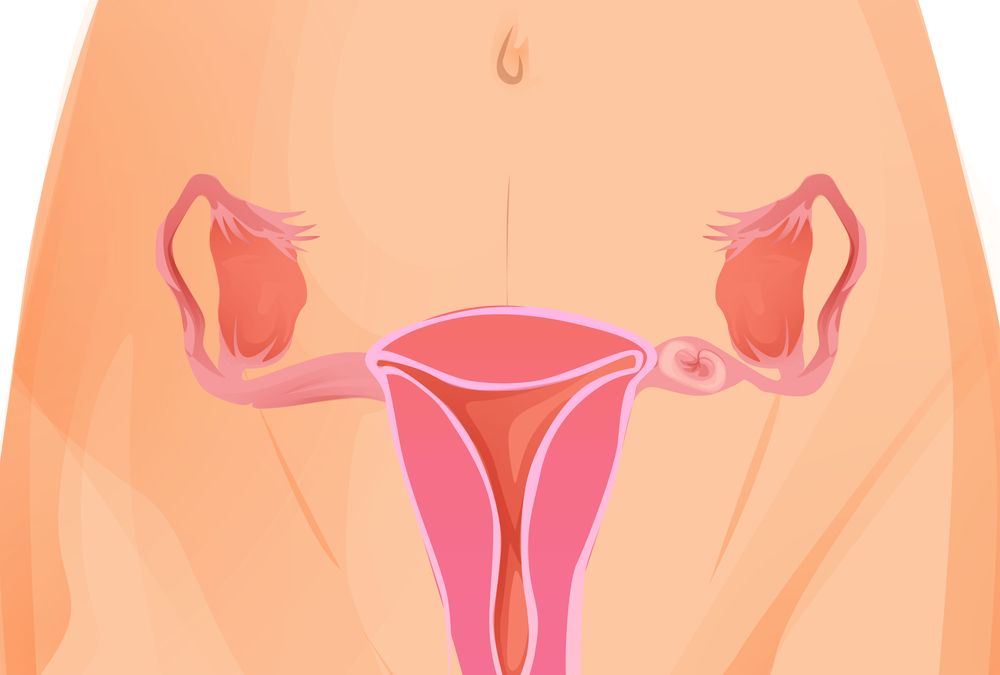
Endometrial cells are cells that line the uterus and are shed during menstruation. These cells can sometimes get stuck in the cervix during the pap smear procedure and appear abnormal under the microscope. Atypical endometrial cells are those that look different from the rest of the pap smear cells (such as having scant cytoplasm or being vacuolated).
These atypical cells can be seen in conventional Pap smears and also in liquid-based pap smears, although they are more frequently observed in liquid-based pap smears. The atypical cells may look different due to their shape or size, or they might have a darker color. Atypical endometrial cells can be a sign of precancerous or even cancerous changes in the uterus, but they are not usually associated with cervical cancer.
Endometrial Cells on Pap Smears: Cytological Correlation with Endometrial Pathology
Many studies have been conducted to examine the correlation between benign endometrial cells in the cervix and endometrial hyperplasia or adenocarcinoma. However, the data is conflicting. For example, some studies have found that the presence of endometrial cells on a Pap test is not associated with subsequent occult atypical or malignant lesions, while others have reported that this is often the case. The interpretation of these findings is complicated by the fact that the threshold for detecting endometrial cells on a pap smear has been lowered over time, making it easier to detect them.
The original 1991 edition of the Bethesda System for Reporting Cervical Cytology recommended that all Pap tests should be reported in postmenopausal women with desquamated endometrial cells. This was based on the idea that these cells carried a higher risk of clinically significant pathology in postmenopausal women than in premenopausal women.
However, the second edition of the Bethesda System (2001) now recommends that all Pap tests be reported in all patients over the age of 40 regardless of whether endometrial cells are present or not. It is also now commonly accepted that the majority of patients over 50 with atypical endometrial cells on a smear do not have underlying endometrial pathology.
In a recent study, Papillo and coworkers38 compared patients with atypical endometrial cells seen on a Pap smear to women without these cells and found that the rate of histologic cervical or endometrial abnormalities was not significantly different between the groups. The authors concluded that this finding suggests that reporting of endometrial cells in all patients over the age of 40 does not lead to a significant increase in histologic detection of premalignant or cancerous lesions.
In addition, a recent study by Karim and coworkers29 included women with benign endometrial cells on their Pap smears that were followed by endometrial histology. This study showed that the women with atypical or malignant histologic findings had, on average, higher numbers of endometrial cells than those with normal results.









