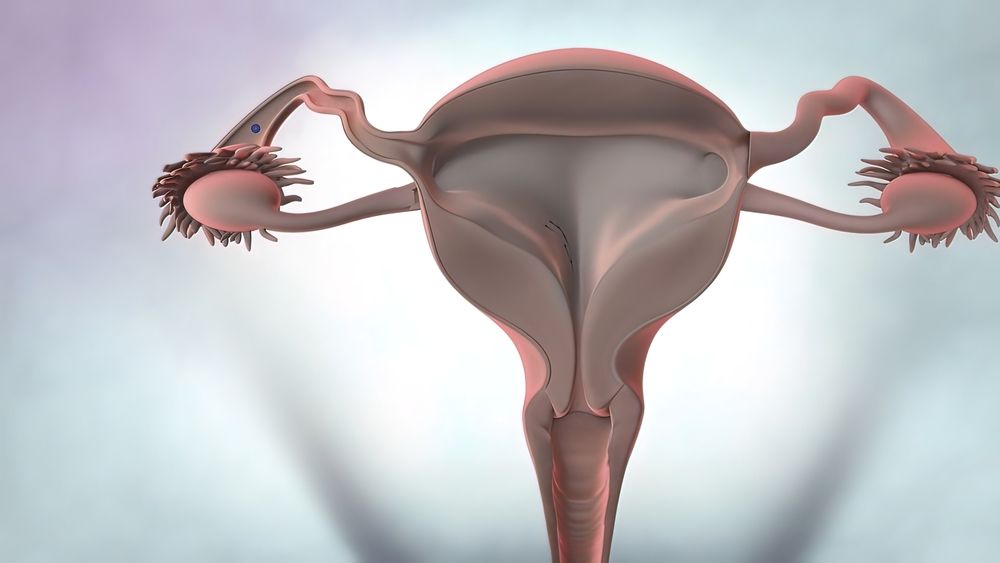
An endometrial polyp is a benign growth found within the uterus. Endometrial polyps differ from uterine fibroids (leiomyomas) in that they originate from the inner lining of the uterus itself while fibroid formation occurs from the uterus’ muscle mass. Polyps are usually found in the top of the uterus and vary in size from millimeters to centimeters. Endometrial polyps occur in women of all ages and are commonly found in patients with abnormal menstrual bleeding, particularly those with a history of pre- or post-menopausal abnormalities. The majority of symptomatic polyps are benign. However, between 2-4% of endometrial polyps will develop pre-cancerous or malignant changes which are not clinically apparent. These changes can be detected on a transvaginal ultrasound, which is routinely performed in most pre- and postmenopausal women with abnormal uterine bleeding.
Most women who have endometrial polyps are unaware that they have them. Typically they are diagnosed when a woman complains of abnormal vaginal bleeding that is heavier than her normal flow and/or a period that happens at a time when she does not expect it. During her gynecologic exam, the physician will perform an ultrasound of the uterus and may also obtain a pelvic smear to check for abnormalities in the lining of the uterus.
When an endometrial polyp is diagnosed, the healthcare provider will review a woman’s medical history to determine any possible risk factors for polyps such as tamoxifen use, obesity and/or family history of cancer. Women who are symptomatic or have had multiple endometrial polyps removed are at an increased risk for developing malignant change in the future.
While no one knows exactly how many women have endometrial polyps, they are thought to be quite common. They are found in up to 39% of women with abnormal bleeding prior to menopause and in 21-28% of women with abnormal bleeding during the postmenopausal period.
Polyps are characterized by areas of “fluffy” endometrial tissue that grow a little too much and then shed, causing a period. They appear on a uterine ultrasound as small, round-shaped spots with a stalk like the trunk of a bush or tree. The polyps’ larger areas are arranged in an “apple core” pattern and may be attached to the stalk.
Polyps can be cured by removing them surgically. A minimally invasive procedure can be used to remove the polyps, which is often done through the cervix. After the procedure, a patient may experience spotting for a few days while the polyps are shedding. After removal, only a small percent of polyps recur. Those that do recur are usually smaller than the original ones and often do not cause any symptoms. The healthcare provider will be able to best advise patients about whether or not polyp removal (called polypectomy) is required. In addition, they will be able to determine if the polyps are in an area of the uterus that should be preserved in order for the woman to become pregnant if she chooses.









