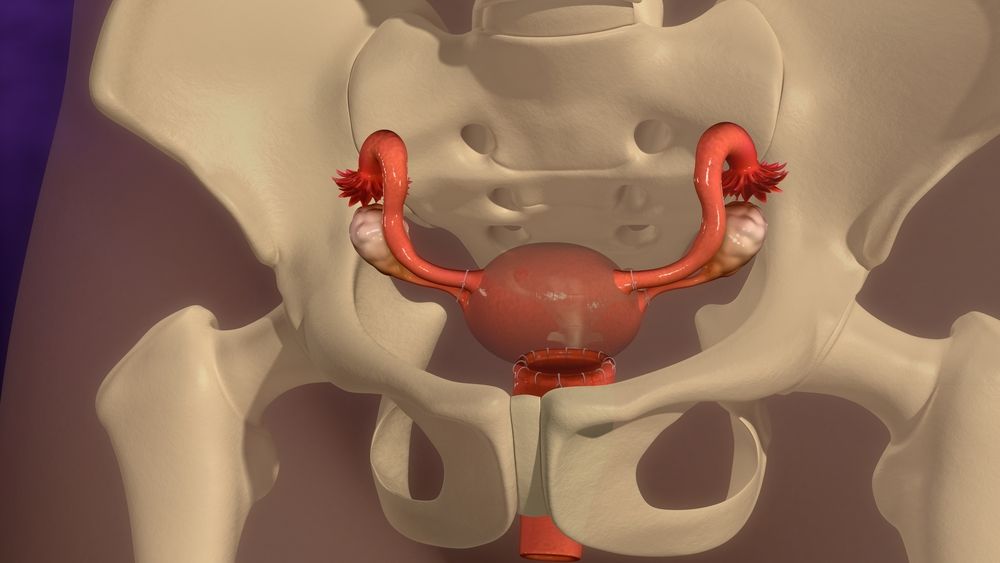
Endometrial stromal sarcoma (ESS) is a rare malignant uterine mesenchymal tumor that develops in the supporting connective tissue of the uterus. The majority of cases occur in premenopausal women and the disease tends to spread to adjacent structures within the pelvic cavity. The symptoms are abnormal uterine bleeding (bleeding that occurs outside of menstruation and after the onset of menopause) and abdominal pain and distension.
Clinical diagnosis of ESS can be challenging because of its nonspecific symptoms and often nondistinctive gross appearance. The tumor is characterized by permeative infiltration of the myometrium and often displays extensive lymphovascular invasion. On radiologic examination, the tumors show a heterogeneous isointensity on T1-weighted magnetic resonance imaging and a homogenous and prominent enhancement on contrast-enhanced MRI. The vascularity of the tumors makes them isointense on T2-weighted images. In addition, a characteristic nodular growth pattern with margins that are thick and indistinct is a distinctive feature of this entity.
In a small number of patients, SS has been shown to have a cytogenetic phenotype and is characterized by a t(7;17)(p15;q21) mutation in JAZF1/JJAZ1 resulting in fusion gene ES-JAZF1. The JJAZ1 fusion protein encodes a chimeric transcription factor and can be identified using break-apart FISH. RT-PCR can also be used to confirm the presence of ES-JAZF1.
The natural history of uterine mesenchymal sarcomas varies widely depending on the cellular grade of the tumor. Low-grade sarcomas have an indolent natural history and can be eradicated with adequate surgery alone, whereas high-grade (also known as undifferentiated) sarcomas are aggressive neoplasms that have a poor prognosis even with adequate surgical resection and systemic treatment.
Although gynecologic sarcomas are relatively rare, it is important for clinicians to be familiar with the different grades of these tumors as they can have very different natural histories. This is especially true for endometrial stromal sarcomas as a large proportion of these tumors have a relatively indolent clinical course with favorable prognosis when appropriately managed.
In this article, we will discuss the salient features that help to distinguish LG-ESS from a more cellular leiomyoma in an endometrial biopsy/curettage specimen and from an aggressive uterine sarcoma with limited infiltration in a hysterectomy specimen. In addition, the differences between LG-ESS and HG-ESS, a tumor recently reintroduced into the WHO classification of uterine sarcomas, will be highlighted as well. We hope that this discussion will allow the gynecologic oncologist to more easily recognize these entities and thus improve patient management. Moreover, this article will serve to increase awareness of this rare mesenchymal neoplasm among gynecologic oncologists and physicians in general. This is particularly important given the rapid enlargement of this tumor at young age and its potential for spreading to surrounding structures within the pelvic cavity. This is not a disease that should be ignored and requires close monitoring of the patient. The use of appropriate imaging modalities is paramount in these patients. In addition, the judicious use of resection techniques and adjuvant therapy is recommended for these patients.









