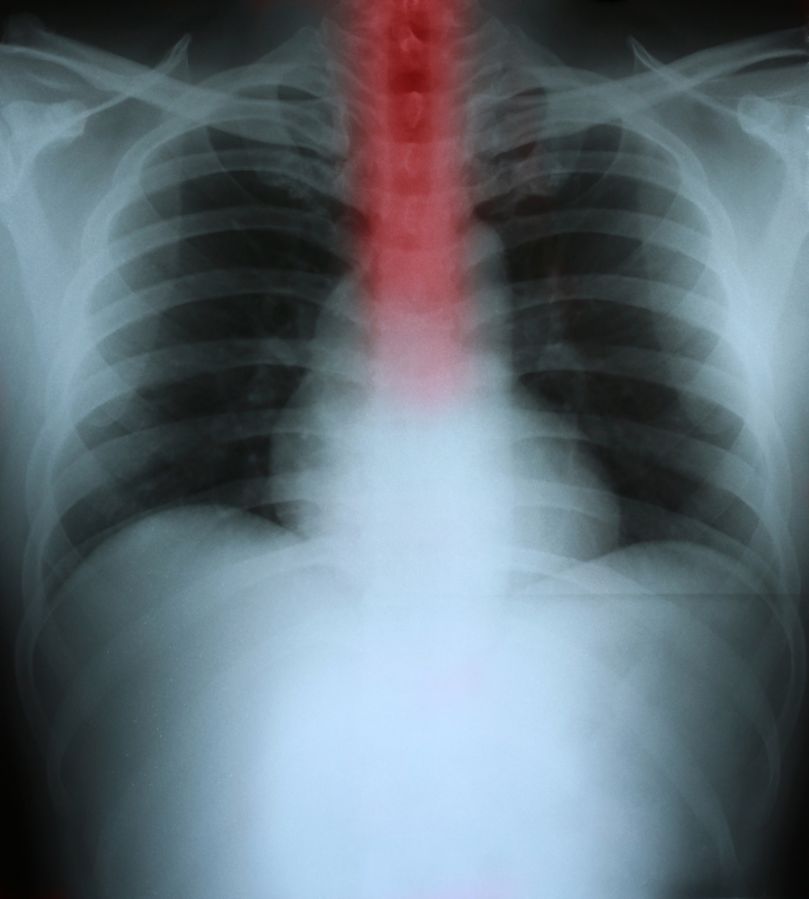
Esophageal adenocarcinoma (EAC) develops in glandular cells that line the esophagus, which is the tube that connects the throat to the stomach. Usually, these cells produce mucus and other substances that help food pass through the esophagus and into the stomach. Cancer starts when the cell’s normal functions are disrupted, often by mutations in genes. Mutations cause the cell to grow, divide, and remain alive longer than it should. Eventually, an overabundance of cells forms a tumor.
If the tumor continues to grow, it may block the esophagus and cause symptoms such as difficulty swallowing, vomiting, and chest pain that occurs a few seconds after eating or drinking. The cancer also can lead to weight loss and dry mouth.
The disease affects primarily middle-aged white men, and its incidence has increased faster than any other cancer in the United States since 1970. It is thought that this increase is due to a rise in gastroesophageal reflux disease (GERD), in which contents from the stomach, including acid and bile, move back up into the esophagus. This can cause chronic inflammation of the esophagus, increasing the risk for adenocarcinoma.
Scientists are working to improve screening tools for esophageal cancer and to develop new treatment options. One goal is to detect adenocarcinoma at an earlier stage, before it has a chance to spread. Another goal is to identify which types of treatments are most effective for a specific type of cancer, so patients can receive the most appropriate care.
There are two main types of esophageal cancer: squamous cell carcinoma and adenocarcinoma. Squamous cell carcinoma begins in the flat cells that line the esophagus, and it can occur anywhere along the esophagus. Adenocarcinoma, which grows from glandular cells that line the esophagus, usually develops in the lower part of the esophagus near the stomach.
The 10th most common cancer in the world, esophageal adenocarcinoma is hard to treat because it spreads rapidly. It is important to get a diagnosis early and to follow up regularly for a recheck of the esophagus, especially in people who have a history of GERD or Barrett’s esophagus, which increases the risk for esophageal adenocarcinoma.