Glioblastoma multiforme (GBM) is the most common and fast-growing type of brain tumor in adults. It is a malignant tumor that spreads throughout the brain and spinal cord, but does not generally spread to other organs. This aggressive and incurable disease kills most people within six months without treatment.
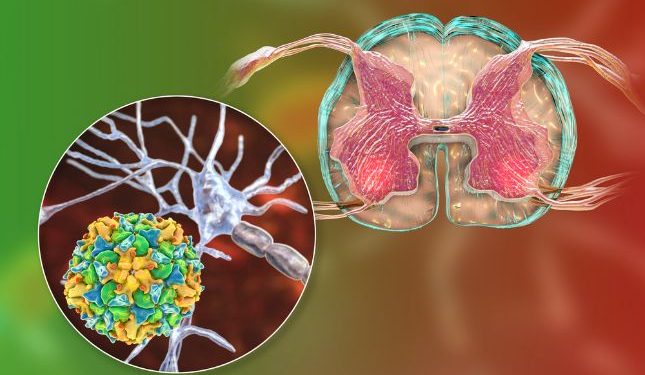
Experts know little about what causes glioblastoma. However, they do know that there is a link between radiation and certain genetic syndromes and a higher risk for developing this cancerous brain tumor. They also know that this cancer usually develops from cells that line the nerve tissue in and around the brain and spinal cord, called glial cell. These tumors are not part of the normal brain tissue and they may form de novo or evolve from lower-grade glial tumors that are found in the brain.
Symptoms of GBM vary depending on the location of the tumor and how rapidly it grows. These symptoms include changes in mental function, memory problems, headaches and nausea. Often, these symptoms are due to increased pressure on the brain from the tumor and shift in intracranial contents. Headaches are a hallmark of GBM and occur in 30-50% of patients (Clarke 2005; Salah Uddin and Jarmi 2015). The headaches are usually unilaterally localized with no specific pattern and may be associated with vomiting and papilledema.
GBMs are usually diagnosed by MRI or CT scan and then confirmed with a biopsy of the tumor. The goal of the biopsy is to obtain a small piece of tumor tissue for testing to look for cancer cells. The biopsy is usually done with a needle that is inserted into the tumor through the skull.

The standard treatment for GBM includes surgery, radiation and chemotherapy. The radiation is usually given as a single dose, but can be delivered in smaller doses over a period of several weeks. The doctor may also use a technique called stereotactic radiosurgery, which uses very precise X-ray beams to target the tumor and limit damage to healthy brain tissue.
Chemotherapy drugs circulate in your blood and destroy the cancerous cells. They are sometimes given with or instead of the radiation, depending on your unique situation. Your provider will use a variety of drugs, including temozolomide and carboplatin. Other treatments include immunotherapy and targeted therapy.
It is important to have regular follow-up after your treatment for GBM. Your healthcare provider will check for signs that the cancer has returned, such as a change on your MRI or an increase in the amount of fluid around your brain (edema). You may have a positron emission tomography (PET) scan if you think the tumor has recurred.
Some people can live for years after they are diagnosed with GBM, but it is important to have regular check-ups and get your MRIs and PET scans regularly so the cancer can be detected early if it recurs. This will help you get the best possible care and improve your chances of survival.