A cell transplant involves replacing unhealthy blood cells with healthy ones. Stem cells are the building blocks of all blood cells and make billions of new blood cells every day to replace old and worn-out ones. Unhealthy blood cells cause many diseases, including cancer and other health problems such as infections, anemia and bleeding. Blood stem cells can be retrieved from the patient’s bone marrow or blood and then infused (transfused) into their body to replace the diseased blood cells. The transplant process is called hematopoietic stem cell transplantation or SCT.
Your child will have several evaluations and appointments before being admitted for a cell transplant, to ensure that they are physically ready for it. These include tests and a review with a senior member of the transplant team. A Stem Cell Transplant patient coordinator will coordinate these appointments and serve as a liaison between your child and the transplant team.
Before the transplant, your child will receive chemotherapy to destroy the diseased blood cells. This pre-treatment treatment can affect your child’s immune system and put them at risk of infections. To help protect your child, they will be in a carefully cleaned room with no physical contact with other people, and they will have medications to prevent infection and to ease nausea, vomiting and diarrhea. They will also have blood and platelet transfusions to keep their levels up, and they will be on medication to reduce the chance of rejection of the transplanted cells.
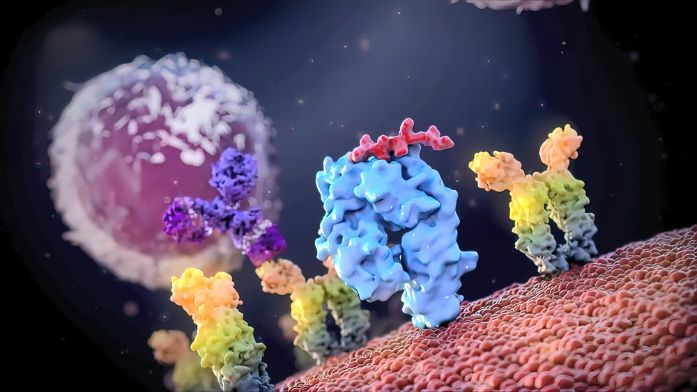
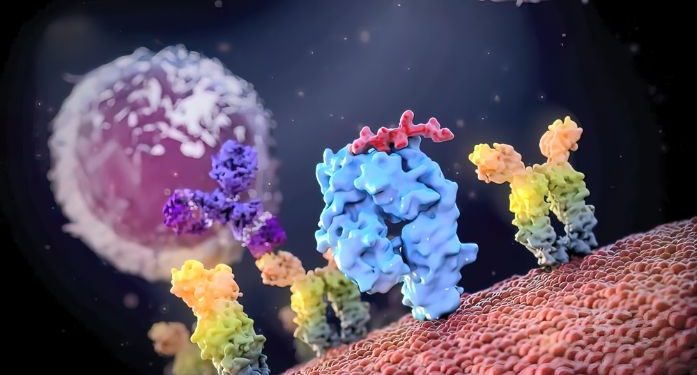
The transplanted stem cells will begin to produce functional blood cells and build a new immune system, a process known as engraftment. They will either come from your child’s own stored stem cells, or they may be donated from another person with closely matched human leukocyte antigens (HLA), like a brother or sister. If the transplanted cells are donated, your child will have a less intensive preparation and conditioning regimen than for an autologous transplant.
If the stem cells are donated, they will be infused into the patient through a thin tube in their chest or neck called a catheter. This tube stays in place through the entire transplant process to give drugs, fluids and blood tests. It reduces the number of needle sticks in the body and allows for better patient comfort.
Scientists are studying stem cells to understand how they work and to develop new ways to treat disease. For example, researchers are using induced pluripotent stem cells (iPSCs) that can be made from a person’s own cells to create small models of organs and tissue chips to test drugs in a safe environment before testing them in people. They are also using these cells to learn more about how cancers develop and grow and to find new treatments for them.