Pancreatitis symptoms vary depending on the severity of the condition. Mild cases usually improve after a few days, while severe cases may require hospitalization for intravenous (IV) fluids and medicines to help with pain relief.
Risk factors for pancreatitis include obesity, diabetes, heavy alcohol use, gallstones in the bile ducts, and certain autoimmune conditions. Having a family history of this disease is another factor that increases your chances of developing it.
The pain caused by pancreatitis usually comes on suddenly and may be more intense after you eat or drink. It can also spread to your back and become constant, sometimes disabling. Other symptoms include nausea, vomiting, a change in your weight and fatty stools that appear oily or have yellow or brown spots (steatorrhea).
People with this condition often lose the ability to taste food. This is because the pancreas is no longer producing digestive enzymes.
A blood test can confirm the diagnosis of acute pancreatitis. It shows how much of the digestive enzymes amylase and lipase are in your blood at the time of the attack. You can have this test at home or in the hospital.
Your doctor may also order an oral glucose tolerance test or a stool test to check how well your body handles sugars. This is done by having you drink a liquid with a little bit of sugar in it and then checking how fast your blood sugar rises afterward.
Treatment depends on the severity of the condition and your medical history. A mild case of acute pancreatitis usually gets better after a few days with rest and treatment, such as dietary changes and medications for pain relief.
For more severe cases of pancreatitis, hospitalization is necessary for intravenous (IV) fluids, pain medication, and nutritional support. Some people will need a feeding tube to help them eat.
During the course of your treatment, you may have other tests to check your kidneys, heart, or lung function. These tests are important to prevent serious complications from developing, such as heart failure or lung disease.
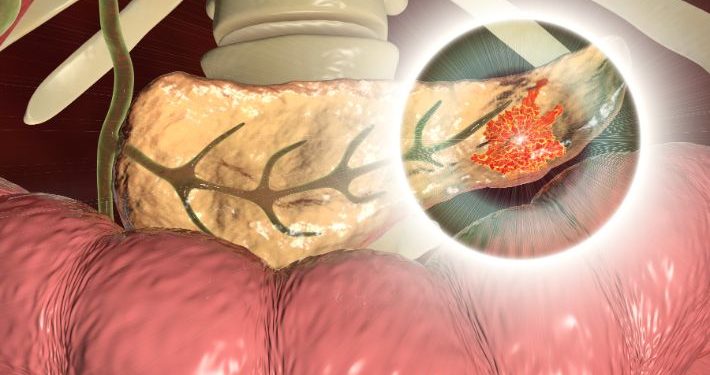
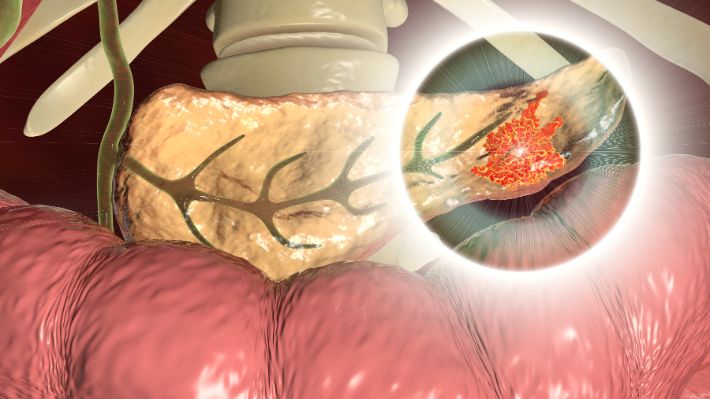
Common tests include a CT scan, ERCP (endoscopic retrograde cholangiopancreatography), and an abdominal ultrasound to look for gallstones. If you have a history of diabetes, your provider may order a blood sugar test.
The cause of your pancreatitis is determined by the results of the tests, along with your medical history and physical exam. It is usually due to damage to the cells that make insulin in your pancreas, although alcohol can cause this condition as well.
You can prevent a severe attack of acute pancreatitis by not smoking, avoiding drinking and alcoholic beverages, and eating small meals that contain no fat. Having an emergency ERCP procedure to remove a blockage in your bile duct or gallbladder can also be helpful.
If the inflammation is not treated, your condition can progress to chronic pancreatitis. This is more serious and may lead to heart failure, pulmonary disease or kidney disease. In some cases, surgery is needed to remove part of the pancreas or other organs that have been damaged by the attack.