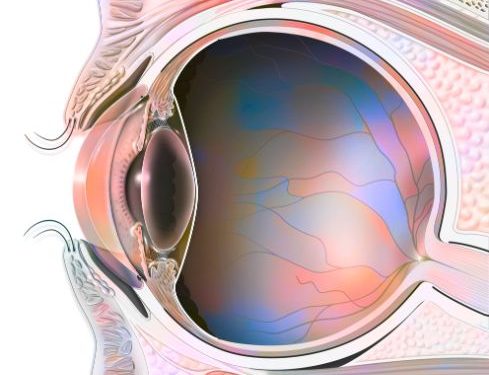
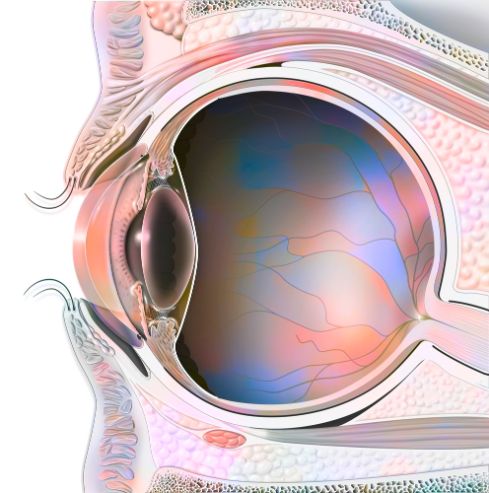
When the gel that fills your eyeball separates from your retina (the back of your eye), it’s called posterior vitreous detachment. Usually this doesn’t cause any problems, but in some rare cases it can lead to an eye problem that needs treatment right away.
Floaters and Flashes of Light
The most common symptom of PVD is floaters, which look like tiny opaque spots or lines that float across your vision. They are a sign that strands of the vitreous have detached from the back of your eye, casting new shadows on the retina.
These floaters can make your vision blurry. They often appear in your peripheral (side) vision and may get worse in dimly lit conditions, such as when you’re outdoors or reading in a dark room.
They may also be seen in your central (front) vision, sometimes forming a Weiss ring.
You can usually tell when you have a PVD by having your eyes dilated with drops to widen your pupil, so that your doctor can see the back of your eye more easily. Your doctor will use a special tool to examine your retina, looking for signs of tears or retinal detachment.
In most people with posterior vitreous detachment, the condition resolves on its own within three months. If you have continued floaters, however, your doctor might recommend treatment that can remove some of the vitreous gel and prevent future floaters.
Detecting Posterior Vitreous Detachment With Dilated Eye Exams
Most people who have a PVD do not need any further treatment because their symptoms disappear within a few weeks. But some patients do develop complications, such as a tear in their retina or a detachment of the macula, which are very serious and must be treated immediately.
A dilated eye exam allows your eye doctor to examine your retina and other parts of your eye with a lighted instrument that is easier to see than the normal light in your eyes. This quick assessment can save your sight and lead to more effective treatment if there’s a more serious eye problem than PVD.
The doctor can also use a non-invasive test to take a picture of your retina using an Optometric Coherence Tomography (OCT) device that uses light rays to create a high magnified, cross-section view on a microscopic level. OCT is a painless procedure that can show small abnormal areas of your retina that would not be seen during an ordinary dilated exam.
During your exam, the doctor will check for retinal tears and traction on the macula, which can happen when the vitreous pulls too hard on the tissue that lines the center of your retina. These tears can be repaired through laser surgery or by removing part of the vitreous gel, known as a vitrectomy.
A retinal tear is more serious than a retinal detachment and can lead to a loss of vision. A retinal tear is most common in older adults, but can happen at any age. It occurs when the liquid vitreous tugs on the tissue of the retina with enough force to break the retina’s underlining tissue. This can cause bleeding in the tissue or a hole or pucker in the macula.