For many men diagnosed with prostate cancer, surgery is an effective treatment option. However, it’s important to understand the potential side effects of this surgery before making a decision.
A physician will review your diagnosis and discuss available options with you. Often, your doctor will recommend a treatment plan that includes the use of both radiation and hormone therapy. These therapies may be used in combination with surgery or given on their own, depending on your individual situation. In some cases, your doctor may suggest a clinical trial or other cutting-edge approach to therapy.
Your doctor will order tests to assess your condition and determine how much prostate tissue is present, which may help to guide the surgical procedure. The most common test is a PSA (prostate-specific antigen) blood test. This measures the amount of prostate-specific antigen in your body and can be an indicator of whether or not your cancer is growing rapidly. Other lab tests, such as a complete blood count and urinalysis, also are useful in assessing your health.
Before your surgery, you will be instructed to stop taking certain medications or supplements that increase your risk of bleeding. This typically includes blood thinners like warfarin (Coumadin) and clopidogrel (Plavix), as well as nonprescription pain relievers such as aspirin, ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve).
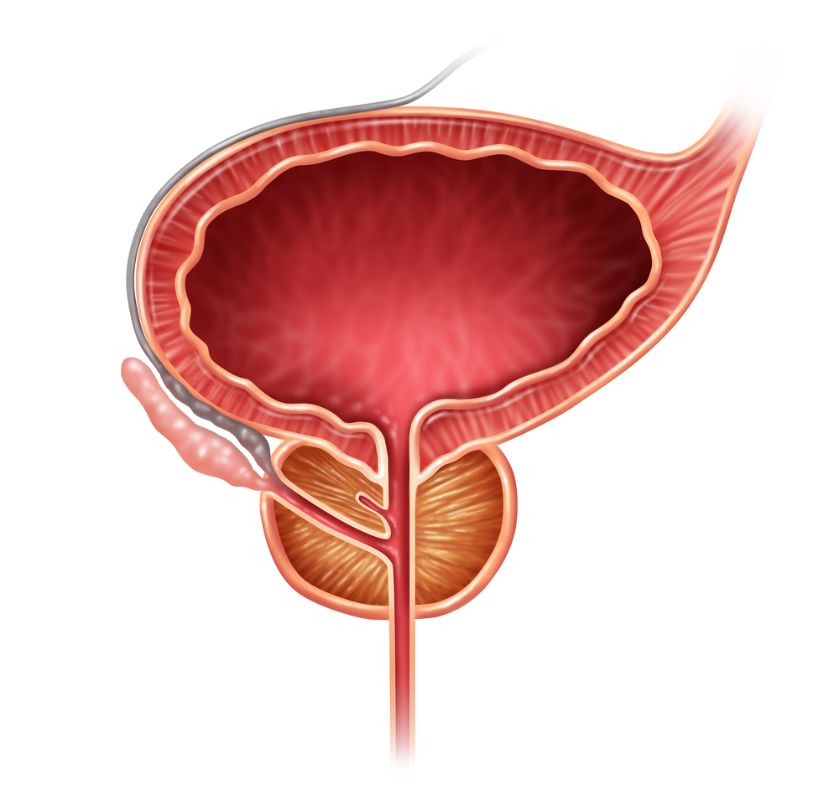
While you are under anesthesia, doctors will make about six small incisions near the rectum to insert instruments. These tools are controlled by a computer console that allows your surgeon to maneuver in places that can’t be reached with a hand. This precision can help to preserve nerves that normally control bladder and sexual function. This type of prostatectomy has a cure rate equal to that of open surgery and can restore normal urinary and bowel functions in most patients.
In some cases, a doctor will need to remove lymph nodes from around the prostate, in addition to the gland. This is usually done if the cancer has spread beyond the prostate, or if your doctor is concerned that it might spread in the future. This type of surgery is called a radical prostatectomy with retropubic approach.
After your surgery, you will need to use a stool softener and laxative on a regular basis. If you are having trouble passing gas or have not had a bowel movement by day three after your operation, you should contact the clinic.
Depending on your surgery, you may have one or two temporary drain tubes placed through punctures near the site of the incision. This helps to prevent urine from building up in the area. Generally, the tubes are removed before you leave the hospital. It’s important to keep the incision and catheter clean and dry. Your doctor will give you specific bathing instructions.
It can take months for normal bladder function to return, especially if you have undergone a radical prostatectomy. A few men lose the ability to control their urine, even with the use of a catheter. If you are concerned about your ability to father children, ask your doctor if you should “bank” sperm before the operation.









