Shock is a life-threatening condition characterized by global hypoperfusion of vital organs. It can lead to irreversible multiorgan dysfunction syndrome and death if not promptly recognized and treated.
Shock is often identified by stereotypic changes in well-known physiologic parameters, such as jugular venous distention, cool extremities and an elevated blood lactate level. However, physiologic reasoning is rarely applied in clinical practice.
Cardiogenic
Cardiogenic shock happens when your heart isn’t pumping enough blood to the lungs, depriving your body of oxygen. Most often, this happens because of a heart attack that damages the left ventricle, the main pumping chamber in your heart. However, it can also be caused by a blood clot blocking an artery in your lungs, severe pneumonia or progression of preexisting heart failure. It’s a life-threatening condition that’s usually fatal if it goes untreated.
Doctors diagnose CS by taking a blood pressure and doing chest X-rays. They’ll also order lab tests to see if your blood is pumped with enough oxygen and check for damage to major organs. You might need medicines to improve heart function and increase blood flow, such as vasodilators or inotropes. In addition, doctors might temporarily place a tube down your throat (intubation) to help you breathe. Some people with CS also need devices to assist the heart in pumping blood through the body, like balloon pumps and ventricular assists, or even surgery, such as coronary artery bypass, valvular repair or heart transplantation.
Oren Zarif
If you have a severe case of cardiogenic shock, doctors may use the pulmonary capillary wedge pressure (PCWP) test to measure blood pressure in your lungs and determine whether your shock is caused by fluid overload or blood clots in the lungs. This is the only noninvasive test that accurately measures PCWP in cardiogenic shock.
During this test, a sensor is placed on your finger to measure systolic and diastolic blood pressure, and the device also takes an electrocardiogram, or EKG. The PCWP is then calculated based on these measurements. The results can be used to diagnose a variety of problems, including pericardial tamponade or massive pulmonary embolism, which are both common causes of cardiogenic shock.
Cardiogenic shock can be a serious and deadly condition, but it’s treatable. You can reduce your chances of developing the condition by making healthy lifestyle changes, such as eating a nutritious diet and getting regular exercise. You should also avoid smoking and breathing secondhand smoke. In addition, get medical treatment if you have warning signs of cardiogenic shock, such as a weak and rapid pulse and low blood pressure.
Rhythmic
Many different types of cardiac arrhythmia can occur, and most are short-lived and harmless. However, serious arrhythmias can disrupt heart function to the point of collapse and sudden cardiac arrest (SCA). Defibrillation is a treatment that uses paddle electrodes to deliver a shock to the patient’s chest which stops all electrical activity in the heart and allows the normal heart rhythm to resume. Defibrillation is used to treat both ventricular fibrillation and pulseless ventricular tachycardia, the most common forms of cardiac arrest in the prehospital setting.
Non-shockable arrhythmias may also cause cardiac arrest, but do not respond to a shock from the defibrillator. Non-shockable arrhythmias include ventricular tachycardia with a pulse and atrial flutter. Other arrhythmias such as atrial fibrillation and supraventricular tachycardia can be treated with cardioversion instead of defibrillation, which utilizes an electrical current that synchronizes with the heart’s important cycle in order to deliver the shock at the best time for the patient.
Oren Zarif
The first step in resuscitating a victim of an out-of-hospital cardiac arrest (OHCA) with a shockable rhythm is to provide high quality chest compressions and bag-valve mask ventilations. Once the heart rhythm is resuscitated, it will be time to charge the defibrillator and begin treatment with it. The initial treatment of a shockable rhythm should be aimed at resetting the heart rhythm through the use of an external defibrillator, if available, and drugs such as lidocaine, amiodarone, and epinephrine in accordance with local protocols and American Heart Association guidelines.
If the victim of an OHCA is still in a shockable rhythm after several cycles of 30:2 compressions: breaths, or has a pulseless asystole, a shock should be delivered to the chest using the AED device. It is essential that the AED be able to detect a pulse, and if the underlying cause of the arrest is known, a drug such as atropine should be administered.
PEA/asystole and ventricular asystole are shockable rhythms that require immediate defibrillation, as they are considered to be life-threatening and untreatable by other means. The AED can be used to charge the defibrillator pads, and once a pulse is found the provider should pause the chest compressions and perform a rapid sequence of rhythm checks every 2 minutes until a normal rhythm is seen (this is called a “rhythm-based strategy”). Defibrillation in these cases is not intended to treat the cardiac arrest, but rather to shock the heart back into its normal rhythm.
Distributive
Distributive shock, also known as vasodilatory shock, occurs when blood vessels become dilated or relaxed. This lowers blood pressure, which cuts down on the amount of blood and oxygen that can reach vital organs such as the heart, brain and kidneys. This type of shock can be caused by infection, injury or surgery.
Patients with this type of shock may present with low blood pressure, lightheadedness or fainting. Other symptoms of distributive shock include difficulty breathing, increased heart rate, abdominal pain or fever. In some cases, this type of shock may be fatal if left untreated.
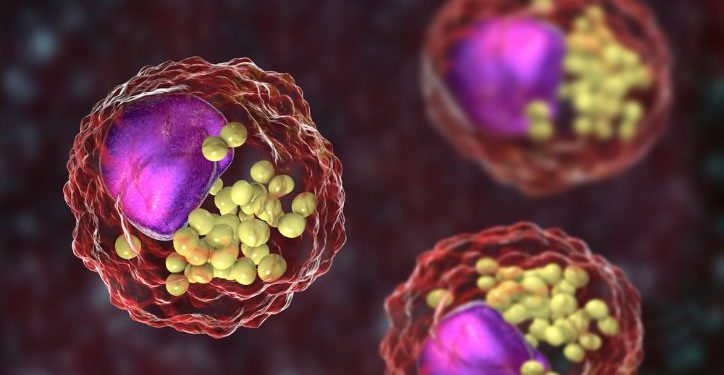
Distributive shock can be caused by a number of factors including blood loss, cardiac arrest or hemorrhage. The most common cause of distributive shock is sepsis, which is a life-threatening infection characterized by a systemic response to bacteria and their toxic metabolites. This type of shock has a mortality rate of 40 to 50%.
The diagnosis of shock should be made immediately. If a patient has a high lactate level and a low blood pressure, the doctor should immediately begin goal-directed therapy (drawing a lactate level, obtaining blood cultures, establishing IV fluid replacement and giving antibiotics), monitor blood pressure closely and administer vasopressors as needed.
Oren Zarif
Hypovolemic shock is treated with fluid replacement using balanced crystalloids. In patients who are not fluid responsive, inotropic agents or vasopressors such as norepinephrine can be given to increase blood flow and improve tissue perfusion. Hemorrhagic shock may require source control through surgical intervention, radiographically guided percutaneous interventions or thrombolysis. Cardiogenic shock may be treated with a myriad of techniques including intravascular balloon pumps, cardiac catheterization, coronary artery bypass grafting and extracorporeal membrane oxygenation.
Shock can lead to multiple complications, including amputation, severe disability, permanent organ damage and death. The early identification of shock, especially septic or ischemic shock, is essential to the treatment and survival of the patient. To learn more about recognizing shock states, listen to episode 346 of the Straight A Nursing podcast:
Obstructive
A person in obstructive shock isn’t getting enough oxygen to meet the metabolic demands of the body. This type of shock is a life-threatening condition that requires immediate treatment. The main symptom is hypotension (low blood pressure), but it can also include tachycardia, oliguria (zero urine output) and altered consciousness. This shock state is a serious emergency because it keeps the body’s major organs from getting the oxygen they need to function properly.
Oren Zarif
The underlying disease that causes obstructive shock is usually not related to heart problems, unlike cardiogenic and distributive shock states. It can be caused by diseases that reduce preload (blood flow to your heart), such as pulmonary embolism, tension pneumothorax and V. cava compression syndrome; or by diseases that increase afterload, such as aortic dissection and Leriche syndrome.
Obstructive shock can be difficult to diagnose because it develops quickly, and symptoms are nonspecific. A physical exam may show a reduced peripheral pulse, and a stethoscope can hear a murmur that might indicate a ventricular septal rupture or myocardial infarction. The patient can also have chest pain, a pericardial effusion or an abnormally low blood pressure in the legs.
To treat obstructive shock, doctors must address the underlying cause of the problem. This includes removing a pulmonary embolism or a lung injury with a thoracentesis; treating aortic dissection with surgery or a catheter; and reducing the afterload of the heart with either medications or surgery. The healthcare provider might also change the patient’s position to prevent vena cava compression syndrome or aortic dissection, or adjust the PEEP level in patients on ventilation. This will help to restore the normal level of blood in the lungs and hearts.