Tuberculous meningitis is a very serious infection that can cause long-term brain damage, even after treatment. It is often fatal, especially in young children and people who have HIV (human immunodeficiency virus).
Symptoms of tuberculous meningitis vary from person to person but are most commonly headaches, fever, loss of appetite, numbness or tingling in the hands and feet, and a change in mental status. In severe cases, patients may have seizures or coma.
TBM has a three-stage clinical course: prodromal, meningitic, and paralytic phases. The prodromal phase is characterized by malaise, headache, low-grade fever, and night sweats. The meningitic phase involves a worsening of symptoms and the appearance of focal neurological signs, such as cranial nerve palsies. The paralytic phase is characterized by a deterioration in neurologic function and progresses quickly to coma or seizure.
In the prodromal phase, the typical patient presents with several weeks of a headache and low-grade fever. These symptoms do not progress in an orderly manner and may be accompanied by night sweats or weight loss.
When the symptoms are more severe, doctors may use MRI or other imaging tests to help diagnose the disease. They may also use antibiotics and other treatments to treat the infection.

The diagnosis of TB meningitis depends on a thorough history, physical exam, and laboratory results. Doctors look for specific findings, such as lymphocytic-predominant pleocytosis in the cerebrospinal fluid and CSF acid-fast bacillus (AFB) smears that are positive.
Other lab tests include blood smears and brain X-rays. They look for certain antibodies to Mycobacterium tuberculosis, and they can tell if the infection is active. They also test for a protein called soluble intercellular adhesion molecule-3 (ICAM-3) and for cytokines and other chemicals that are released by the body to fight infections.
Using a scoring system that assigns severity to a symptom, doctors can determine how serious a patient’s symptoms are. The score ranges from 3 to 11, with 1 being mild and 11 being very serious.
If the score is 4 or 5 it means that you have a high chance of dying from the infection. If the score is 6 or more it means that you have a good chance of survival if the treatment is started quickly.
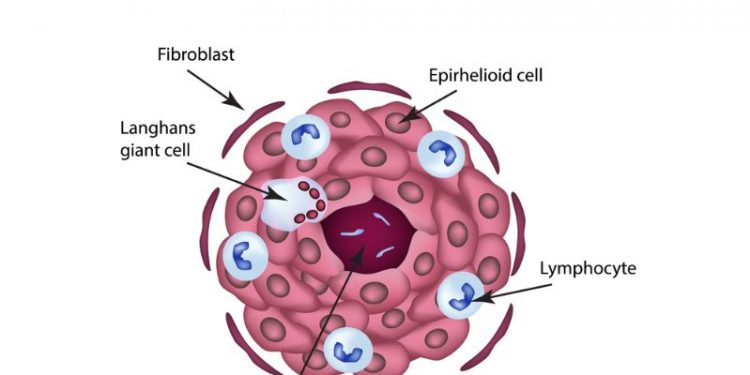
The underlying pathogenesis of tuberculous meningitis is complex and includes both bacterial and inflammatory processes that occur in the central nervous system (CNS). In the lungs, the infection is caused by Mycobacterium tuberculosis, while in the brain, the bacilli produce granulomatous inflammation.
Because of this complex inflammatory process, the meninges may become inflamed and swollen. This causes swelling of the cerebrospinal fluid and a buildup of pressure in the brain. This leads to brain damage and a poor outlook.
Treatment of tuberculous meningitis typically starts with antibiotics, which can kill the TB bacteria. Doctors also prescribe anti-inflammatory drugs and steroids. These can reduce the swelling and pain of the meninges, which is an important part of the treatment. They can also prevent a stroke or other complications from developing.