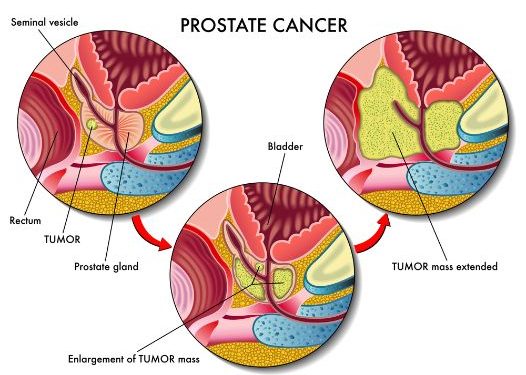
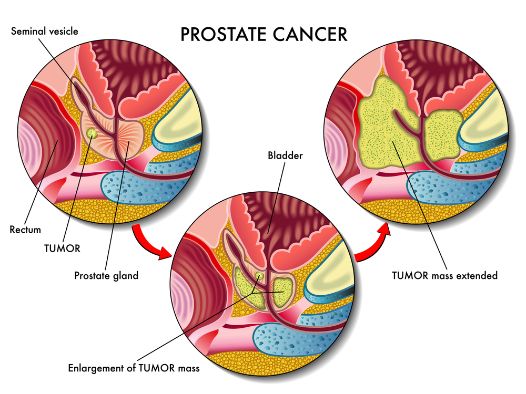
Radical prostatectomy is the surgery to remove the prostate gland, seminal vesicles and, in some cases, nearby lymph nodes, after a diagnosis of localized prostate cancer. It is one treatment option for men with cancer that has not spread beyond the prostate and who have a reasonable expectation of living at least 10 more years.
Patients and their physicians need accurate information about the range and patterns of complications that can occur after radical prostatectomy. However, there are limited data from unselected population-based cohorts.
In this study, we used data from the National Cancer Institute of Canada Clinical Prostate Disease Outcomes Database to assess urinary and sexual function 1 or more years after radical prostatectomy for clinically localized prostate cancer. We examined the effects of a wide range of surgical approaches and of tumor stage on functional outcomes.
The results show that overall, the rate of incontinence and impotence after radical prostatectomy is low. The rates of these problems vary widely according to the type of surgery, including whether it is done with or without nerve sparing (an approach that tries to preserve the nerve bundles that control erectile function). Urinary and sexual function returns to near normal levels in most men, but it can take weeks or months.
Most men have mild to moderate pain after surgery, which is controlled with prescription pain medications. Some may need a drain tube inserted through puncture wounds in the skin, with one tube going into the bladder and the other into the area where the prostate was removed (pelvic drain).
UCSF offers robotic prostatectomy using the da Vinci robot system, which provides excellent magnification and surgical precision. The surgeon makes five small incisions in the lower abdomen through which a robot-controlled camera and arms are passed to perform the procedure. The surgeon operates a console, which is attached to the robot system, to direct its movements.
We also offer extraperitoneal laparoscopic radical prostatectomy, which is an alternative to the open RRP. In this technique, the urethra is disconnected from the bladder, and the surgeon makes an incision in the belly. The bladder is then connected to the urethra, and the scrotum is reattached to the anus.
The incisions are very small, and the surgeon can see everything on a video monitor, so this method minimizes blood loss and tissue damage. A small number of men need to stay in the hospital for a few nights, but most can go home on the same day. We encourage you to ask questions and take notes, and to have someone with you to help remember the information given to you after your operation. Your doctor will provide written instructions and advice on your recovery, including diet, exercise and home care. We will remove the bladder and prostate drainage tubes before you go home, but you will still have a catheter in your urinary tract for several days or longer. Follow-up appointments are important to make sure the cancer has not returned or is growing less quickly.