In the final weeks of life, people with cancer experience physical and emotional changes. These can be upsetting for family and friends. But knowing what to expect can help. Marie Curie nurses Maria, Peter and Shital explain the common changes people may notice in the last weeks and days of their lives and share their own experiences.
It’s important to discuss your end-of-life plan with your doctor. Your doctor will be able to give you a realistic picture of your chances of responding to further treatment and how it might affect your quality of life. It’s also important to talk about the impact of any other health conditions you may have.
For some patients, the best option at this stage is observation or watchful waiting. This means your care team will monitor the cancer and intervene with treatment if it starts to grow or cause symptoms. This is the case for some people with prostate cancer at stage 4, for example.
If the cancer hasn’t spread too far, your care team might recommend surgery to try to remove the tumours and reduce your symptoms. For some types of cancer, such as cervical cancer, you might need a hysterectomy and removal of nearby lymph nodes (a procedure called a radical hysterectomy). If the cancer has spread to your bladder or back passage (rectum), your care team may suggest radiotherapy.
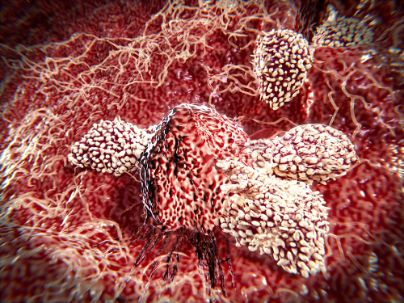
Your care team will also consider the possibility of chemotherapy to improve your quality of life. This is a treatment that can shrink tumours and ease pain, nausea, fatigue and breathlessness. But it’s important to remember that it can’t cure your cancer – it can only help control your symptoms.
Some people may not be able to eat much at this point because the cancer has stopped their stomach working properly. This is sometimes called ascites. If you have ascites, your care team might put a tube into your lower tummy to drain off the fluid under an anaesthetic.
It’s common for cancer to make your tummy swell. Your care team will help you eat small meals as often as possible to get the nutrition you need. They might also use a tube to drain any fluid that builds up in your tummy.
As your cancer progresses, you might feel tired and drowsy more and more frequently. This is because your body is using all of its energy to fight the cancer. You might also have side effects, such as a dry cough or breathlessness that makes it hard to breathe.
It’s important to be honest with your loved ones about how you’re feeling. If you’re finding it difficult to express your emotions, you might find it helpful to write them down in a journal. You can also ask your care team for support to help you talk about how you’re feeling. They can offer you practical tips, such as a warm blanket or music to help you relax. They can also refer you to a palliative care specialist who can help with your emotions and provide support.








