Most womb cancers start in the cells that line the womb (endometrium). It’s also possible for womb cancer to begin in the muscle tissue surrounding the uterus. These are called uterine sarcomas and are treated in a slightly different way. Womb cancer is the fourth most common type of cancer in women. It usually occurs in women and people who have gone through the menopause, but it can affect anyone who has a womb.
The most common symptom is abnormal vaginal bleeding, especially after the age of 50. The bleeding is usually heavier than a normal period, and it may occur more frequently or be accompanied by other symptoms. If you have these symptoms, visit your GP as soon as you can. Your GP will examine you, and they may refer you to a specialist.
Abnormal vaginal bleeding is the main symptom of womb cancer, but it can also be a sign of other conditions that affect the womb, such as fibroids. You should always tell your GP about any unusual vaginal bleeding, regardless of its cause.
If your GP suspects that you might have womb cancer, they will carry out further tests to work out the stage of the tumour and how it has spread. These tests can include an ultrasound scan of your womb and the pelvic area, blood tests to check for cancerous cells, and a biopsy of your womb lining or a sample of the tissue that lines it (endometrium). The results of these tests will help your doctor decide what treatment you need.
Your GP will discuss the results of the tests with you. They will talk to you about the chances of surviving the cancer, and how it might affect your quality of life. This is called palliative care.
Some things are thought to increase your risk of womb cancer, including being overweight, taking hormone replacement therapy after the menopause, and having a family history of breast or ovarian cancer. It isn’t always possible to prevent womb cancer, but the risk can be reduced by maintaining a healthy weight and using some types of contraception.
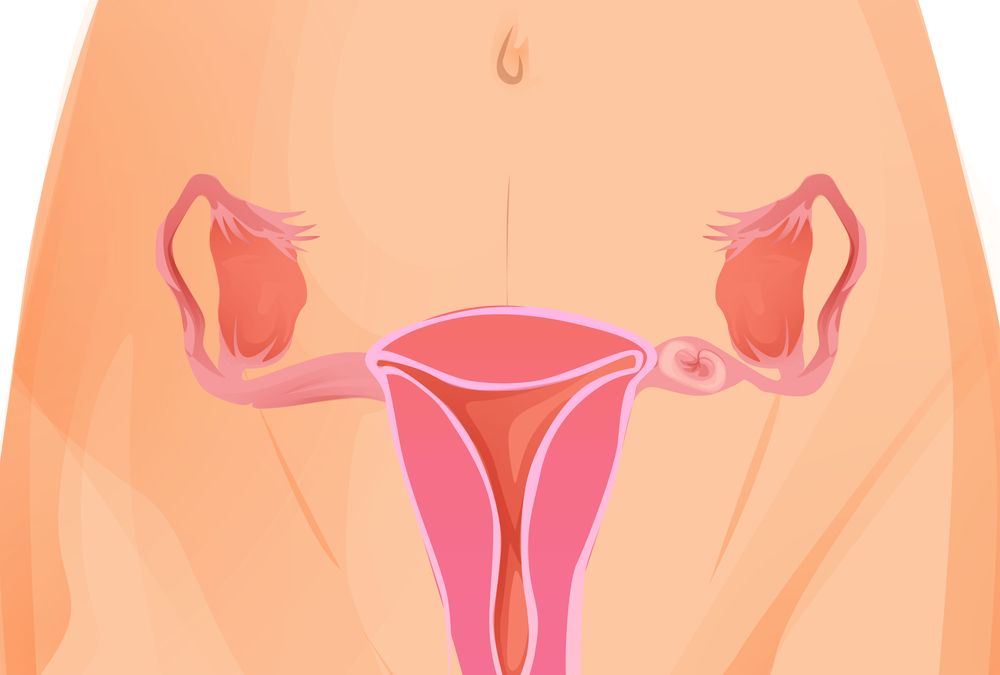
The most common treatment for womb cancer is the surgical removal of your womb (hysterectomy). It’s likely that the surgery will also involve removing your ovaries and fallopian tubes. Sometimes radiotherapy or chemotherapy(external links open in a new window / tab) is used, usually alongside surgical treatment.
You might be offered the chance to take part in a clinical trial to test new treatments for womb cancer. This isn’t always available for everyone, but it’s worth talking to your GP about what options might be open to you. You can change your mind at any time. You can read more about deciding whether to take part in a clinical trial(external link opens in a new window / tab). It’s important that you understand the risks and benefits of taking part in one.









